Unit Compilation 3
Ch.5
the Skeletal System
Table of
Contents
5.1 The skeletal system consists of connective
tissue
a. Bones are the hard elements of
the skeleton
b. Bone contains living cells
c. Ligaments hold bones together
d. Cartilage lends support
5.3 Mature bone undergoes remodeling and repair
a. Bones can change in shape, size,
and strength
b. Bone cells are regulated by
hormones
c. Bones undergo repair
5.4 The skeleton protects, supports, and permits
movement
a. The axial skeleton forms the
midline of the body
1. The skull: Cranial
and facial bones
2. The vertebral column:
The body’s main axis
3. The ribs and sternum:
Protecting the chest cavity
b. The appendicular skeleton:
Pectoral girdle, pelvic girdle, and limbs
1. The pectoral girdle
lends flexibility to the upper limbs
2. The pelvic girdle
supports the body
5.5 Joints form connections between bones
a. Joints vary from immovable to
freely movable
b. Ligaments, tendons, and muscles
strengthen and stabilize joints
5.1 The skeletal
system consists of connective tissue
The
skeletal system is made up of three types of connective tissue:
1.
Bones-
the hard elements of the skeleton
2.
Ligaments-
bind bones together
3.
Cartilage-reduces
friction in the joints
Here is a
picture of a knee joint that shows all three types of connective tissue.
5.1a Bones are
the hard elements of the skeleton
Bones consist of
living cells surrounded by extracellular deposits of calcium minerals. Bones
store minerals and produce cellular components of blood (Red Blood Cells, White
Blood Cells and Platelets). The mass of bones, which consists of nonliving
extracellular crystals of calcium minerals, is what gives bones their hard,
rigid appearance and feel (Johnson 2012).
Bones have five important functions (Oellers, Online
Presentation, 2012):
1.
Support
soft internal organs like the lungs, liver and spleen.
2.
Protects
the soft internal organs.
3.
The
attachment of our bones to muscle is what makes it possible for us to move.
4.
Blood
Cell Formation- cells in certain bones are the only source of new red and white
blood cells and platelets for blood. Without this production we would die.
5.
Mineral
Storage of Calcium and Phosphate bones store these two important minerals.
5.1b Bone
contains living cells
Bones structure
is made up of a hard inorganic matrix of calcium salts (Oellers, Online
Presentation, 2012).
Bone is classified as either compact or spongy.
Compact bones form the shaft, cover each end (epiphysis) of the bone and contain
yellow bone marrow in the central cavity in the shaft (diaphysis). Yellow bone
marrow is primarily fat that is used for energy. A tough layer of connective
tissue, the periosteum, which
contains specialized bone-forming cells, covers the outer surface of the bone.
Inside each epiphysis is spongy bone. Compact bone is made up largely of
extracellular deposits of calcium phosphate, surrounding living cells called osteocytes (mature bone cells).
Osteocytes are
arranged in rings in cylindrical structures called osteons (haversian system).
Osteocytes near
the center of an osteon, receive nutrients by diffusion from blood vessels that
pass through a central canal (Haversian canal). Haversian canals are also
called central organs (Oellers, Online Presentation, 2012).
As bone develops
and becomes hard the osteocytes become trapped in hollow chambers called lacunae (Johnson 2012). The osteocytes
remain in direct contact with each other by thin canals called canalicule. Within the canaliculi, gap
junctions join extensions of the cells cytoplasm of adjacent osteocytes
together (Johnson 2012). Gap junctions are
channels that permit the movement of ions, water, and other molecules between
two adjacent cells (Johnson 2012). Osteocytes are supplied with nutrients by
the exchange of nutrients across this gap junction, even though most osteocytes
are not located near a blood vessel. Waste products produced by the osteocytes are
exchanged in the opposite direction and are removed from the bone by the blood
vessels (Johnson 2012).
Spongy bone is less dense than compact bone,
allowing bones to be light and strong. Spongy bone is composed of calcium
minerals and living cells that are strong trabreculae
(little beams). An example of spongy bone is the upper arms and legs (the
humerus and femur). The spaces between the trabeculae in the upper arms and
legs are filled with red bone marrow,
which is responsible for the production of red and white blood cells and
platelets.
5.1c Ligaments
hold bones together
Ligaments attach bone to bone (Johnson 2012).
Ligaments are comprised of connective tissue (closely packed collagen fibers
oriented in the same direction with a few fibroblasts in between) that holds
bones together. Fibroblasts are
cells that produce and secrete the proteins that compose collagen, elastic, and
reticular fibers (Johnson 2012). Ligaments give strength to certain joints,
while still allowing movement of the bones in relation to each other. When
damaged, ligaments are slow to heal because they have very few living cells and
a poor blood supply.
5.1d Cartilage
lends support
Cartilage contains fibers of collagen or elastin
in a ground substance of water and other materials (Johnson 2012). Cartilage
needs to be flexible to support the joints under pressure when movement is
necessary. In a moveable joint, bone surfaces are covered by a layer of smooth
cartilage and lubricated with fluid, to reduce friction and wear (Johnson
2012).
There are three types of cartilage:
1.
Fibrocartilage mainly made up
of collagen fibers arranged in thick bundles. Fibrocartilage allows the joints
to withstand pressure and tension well. Example of a joint made up of
fibrocartilage is the knee joint called the menisci.
2.
Hyaline
cartilage
is smooth, almost grassy. Hyaline cartilage is thin collagen fibers (Johnson
2012). This type of cartilage forms the embryonic structures that later become
the bones and covers the ends of mature bones in joints to create a smooth,
low-friction surface.
3.
Elastic
cartilage
is made up of elastin fibers. This type of cartilage is very flexible and aids
in forming the outer ear and to the epiglottis (a flap of tissue that covers
the larynx during swallowing) (Johnson 2012).
5.3 Mature bone undergoes remodeling and repair
Bones change
throughout one’s lifetime. Bone is a dynamic tissue that undergoes constant
replacement, remodeling, and repair (Johnson 2012).
A bone called an
osteoclast is a bone-dissolving cell.
This cell remodels and repairs injured bones by dissolving bone when the bone
needs to be renewed and allows new cells to form. This cell cuts through mature
bone tissue, dissolving the hydroxyapatite
(calcium phosphate (Oellers, Online Presentation, 2012)) and digesting the
osteoid matrix in their path. This means that when a bone is fractured or
injured the bone is now curved and misshaped. Over time bone is deposited on
the inside curvature and removed by osteoclasts from the outside curvature. This
result in a bone matched to its previous shape.
Osteoclasts
and the Mechanism of Bone Resorption. A: Light micrograph and B: electron
micrograph of an osteoclast, demonstrating the ruffled border and numerous
nuclei. C: Osteoclastic resorption. The osteoclast forms a sealing zone via
integrin mediated attachment to specific peptide sequences within the bone
matrix, forming a sealed compartment between the cell and the bone surface.
This compartment is acidified such that an optimal pH is reached for lysosomal
enzyme activity and bone resorption.
http://www.endotext.org/parathyroid/parathyroid1/parathyroid1.html,
Retrieved April 10, 2012.
5.3a Bones can change in shape, size and strength
If constant
remodeling is done repeatedly, this can affect the shape of a bone. Electrical
currents stimulate the bone-forming osteoblasts caused by repeated compression
stress on a bone such as jogging.
Having dense,
stronger bones will help in reducing bone injuries. Having a regular program of
any weight-bearing exercise such as weight lifting will increase your muscular
strength. Osteoporosis is a bone disorder that can cause the bone to become
brittle and fracture easily. Science Daily (April 25, 2012) wrote an article
that says research shows that osteoporosis results from hundreds of genes, although
body weight, build and gender play a role as well. Researchers are now trying
to develop an anti-osteoporosis drug.
Homeostasis is important in bone structure and depends
on the balance of osteoclasts and osteoblasts.
Osteoporosis is a result of losing bone mass due to an imbalance of
osteoclasts and osteoblasts.
5.3b Bone cells
are regulated by hormones
These hormones are:
·
Parathyroid
(PTH) removes
calcium from bone. PTH stimulates the osteoclasts to secrete more bone
dissolving enzymes when blood levels of calcium fall below a given point.
·
Calcitonin adds calcium to
the bone if calcium levels rise. Calcitonin stimulates osteoblast activity
causing calcium and phosphate to be removed from blood and deposited in bone
(Johnson 2012).
5.3c Bones
undergo repair
When your break or fracture a bone the blood vessels supplying the bone bleed into the area, producing a mass of clotted blood called a hematoma (Johnson 2012). The repair process begins when fibroblasts become chondroblasts (cartilage forming cells laid down first, then the osteoblasts which are young bone forming cells) and together they produce a tough callus (formed of protein and cartilage) formation between the two broken ends of the bone. The osteoclasts begin to remove dead fragments of the original bone and the blood cells of the hematoma. The osteoblasts then deposit osteoid matix converting the callus into bone. The repair process can take weeks to months depending on a person’s age.
5.4 The skeleton protects, supports, and permits
movement
The human body has 206 bones and the connective tissues that hold them together make up the skeleton.
Bones can be classified into four types based on shape:
1.
Long bones are cylindrical
with growth heads. The epiphysis is at either end and the long bone is covered
by articular cartilage. Long bones include the limbs and fingers.
2.
Short bones are cube shaped
with movements that are more complex. They include the wrist bones.
3.
Flat bones protect the
internal organs and include the skull, ribs, scapula (shoulder blade), sternum
(breastbones) and pelvic girdle (Oellers online presentation 2012).
4.
Irregular bones include shapes
that do not fit into the other categories such as the hip, vertebra and some
facial bones.
http://www.google.com/#hl=en&sclient=psy-ab&q=diagram+of+a+cut+through+a+long+bone&oq=diagram+of+a+cut+through+a+long+bone&aq=f&,
Retrieved April 12, 2012.
1.
It
is the structural framework for support of the soft organs.
2.
It
protects certain organs from physical injury for example the brain is enclosed
within the bones of the skull, and the heart and lungs are protected by a bony
cage consisting of ribs, sternum and vertebrae (Johnson 2012).
3.
The
way that the bony elements of the skeleton are joined together at joints,
permits the body to move like the hands, feet, legs and arms.
The skeleton is
organized into the axial skeleton and the appendicular skeleton
5.4a The axial skeleton forms the midline of the body
The axial skeleton is the skull, sternum, ribs and vertebral column (Johnson 2012).
5.4a, 1 The
skull: Cranial and facial bones
The skull
consists of approximately two dozen bones that protect the brain and form the
structure of the face (Johnson 2012). The cranial bones are flat bones in the
skull that enclose and protect the brain. Starting at the front of the skull
are the frontal bone that makes up
the forehead and the upper ridges of the eye sockets. At the upper left and
right sides of the skull are the two parietal
bones, the two temporal bones
are the lower left and right side that is has an opening into the ear canal for
sound to travel to the eardrum. The facial bones compose the front of the
skull. On each side of the nose are the two-maxilla bones, which form part of the eye socket and contain the
sockets that anchor the upper row of teeth. The sphenoid bone is in between the frontal and the temporal bones. The
sphenoid bone forms the back of both eye sockets. The ethmoid bone contributes to the eye sockets and supports the nose.
The nose is made up of cartilage and other connective tissue. The nasal cavity
is the part of the space formed by the maxillary and nasal bones. The nasal bones are beneath the upper
bridge of the nose only. The lacrimal
bones at the inner eye sockets have tiny openings so tear ducts can drain
tears from the eye sockets into the nasal cavity. The mandible or lower jaw contains sockets that house the lower row of
teeth and attaches to the temporal bone by a joint so that the jaw is able to
move allowing us to talk and chew. The occipital
bone curves underneath to form the back and base of the skull. The foramen magnum is a large opening near
the base of the occipital bone. This is where the vertebral column connects to
the skull and the spinal cord enters the skull to communicate with the brain.
Several of the
cranial and facial bones contain air spaces called sinuses, which make the skull lighter and give the human voice its
characteristic tone and resonance. Each sinus is lined with tissue that
secretes mucus, a thick, sticky fluid that helps trap particles in the air. The
mucus then drains into the nasal cavity by small passageways.
http://en.wikipedia.org/wiki/Vertebral_column,
Retrieved April 10, 2012.
The vertebral column is the main axis of
the body (Johnson 2012). It supports the head, protects the spinal cord and
serves as the site of attachment for the four limbs and various muscles.
1.
The Cervical which contains
seven vertebrae
2.
The Thoracic which contains
twelve vertebrae
3.
The Lumbar which contains
six vertebrae
Vertebrae share
two points of contact called articulations
located behind their main body. The vertebrae are separated from each other by
flat, elastic, compressible intervertebral disk composed of a soft gelatinous
center and a tough outer layer of fibrocartilage (Johnson 2012). Intervertebral disks act as shock
absorbers, protecting the vertebrae from the impact of walking, jumping and
other forms of movement.
A slipped disk
or herniated disk happens when we
make a sudden movement. This kind of movement forces the intervertebral disk
outward, pressing against spinal nerves that result in intense back pain. If a
disk ruptures, surgery can be performed to remove the damaged disk however;
spinal flexibility will be decreased.
5.4a, 3 The ribs
and sternum: Protecting the chest cavity
http://www.daviddarling.info/encyclopedia/R/rib-cage.html,
Retrieved April 10, 2012.
Humans have 12 ribs. One end of each rib branches from the chest cavity (thoracic region) and the other end attach to the sternum or breastbone by cartilage. The breastbone is a flat blade shaped bone composed of three separate bones that fuse together during development (Johnson 2012). The bottom two pairs of ribs are called floating ribs because they do not attach to the sternum at all.
The ribs,
sternum and vertebral column form a protective rib cage that surrounds and
protects the heart, lungs and other organs of the chest. The rib cage helps us
breathe because the muscles between the ribs lift them slightly during
breathing, expanding the chest cavity and inflating the lungs.
5.4b The
appendicular skeleton: Pectoral girdle, pelvic girdle and limbs
http://disciplineorregret.com/?p=1998,
Retrieved April 10, 2012.
The pectoral girdle, the pelvic girdle and the limbs make up the appendicular skeleton the second division of the human skeleton. These parts of the body are called appendages. The pectoral girdle consists of the shoulder, clavicle (collar bone) and scapulas (shoulder blade), the pelvic girdle consists of the hips (coxal bones), sacrum (pelvis) and pubic symphysis, limbs consist of femur (upper leg), tibia (lower leg, inside), fibula (lower leg, outside), ankle and foot bones.
5.4b, 1 The
pectoral girdle lends flexibility to the upper limbs
The pectoral girdle is the supportive framework for the upper limbs, which consists of the right and left collarbones and the right and left shoulder blades.
The arms and
hands consist of 30 different bones (Johnson 2012).
The upper end of the humerous (upper arm, the long bone) fits into the shoulder blade socket, while the other end of the humerus meets with the ulna (forearm, short bone, inside) and radius (forearm, long bone, outside).
The ulna and the
radius are the two bones of the forearm at the elbow. When you hit your “funny
bone” or elbow you actually struck the ulnar
nerve that travels along the elbow.
The lower ends
of the forearm bones meet the carpal
bones (wrist bones), a group of eight bones that make up the wrist. The
five metacarpal bones form the palm
of the hand and they join with the 14 phalanges,
which form the fingers and thumb (Johnson 2012).
The pectoral girdle and arms have a wide
range of motion that provides the upper body a greater range of motion than any
other joint in the body. The pectoral girdle and arms connect to the rest of
the body by muscles and tendons that are attached loosely to provide a greater
range of motion. However, the more flexibility you have the greater your
chances are of falling because of instability. This can lead to fractured or
broken bones. The collarbones are the most frequent broken bones in the body.
Having a wide range of motion allows us to easily excel in sports such as tennis, but repetitive motions such as swinging the tennis racket repeatedly can lead to health problems called repetitive stress syndromes. A well known repetitive stress syndrome is a condition of carpal tunnel syndrome a condition often due to repetitive typing (Johnson 2012).
5.4b, 2 The
pelvic girdle supports the body
The pelvic girdle consists of the two coxal bones (hips) and the sacrum (pelvis) and coccyx (tailbone) of the vertebral column (the last four vertebrae that are fused together toward the pelvis). The pelvis is formed by the hip bones that attach to the sacral region of the vertebral column in the back, then curve forward to meet in front at the pubic symphysis, where they are joined by cartilage (Johnson 2012).
The primary
function of the pelvic girdle is to support the weight of the upper body
against the force of gravity and to protect the organs inside the pelvic cavity
and serve as a site of attachment for the legs (Johnson 2012).
The lower limbs
of the pelvic girdle have a less range of motion than the upper body of the
pectoral girdle because the lower limbs are firmly connected to the rest of the
body limiting dexterity.
The pelvic
girdle is broader and shallower in women than men, mainly due to women being
able to have a baby pass through the birth canal safely. The changes in the
pelvic girdle becomes noticeable in women during puberty, when the women’s body
begins to produce sex hormones that trigger a process of bone remodeling and
shapes the female pelvic girdle to adapt for pregnancy and birth.
The femur (thighbone) is the longest and
strongest bone in the body (Johnson 2012). The rounded upper end of each
thighbone fits securely into a socket in a hipbone, creating a stable joint
that supports the body, while moving. The lower end of the femur intersects at
the knee joint with the larger of the two bones of the lower leg, the tibia (lower leg), which in turn makes
contact with the thinner fibula
(lower leg) (Johnson 2012). The patella
(kneecap) is a triangle-shaped bone that protects and stabilizes the knee
joint. At the ankle, the tibia and fibula join with the seven tarsal bones that make up the ankle and
heel. Five long bones, the metatarsals, form the foot. The 14 bones of the
toes, like those of the fingers, are called phalanges.
5.5 Joints form connections between bones
Joints,
ligaments and tendons hold the skeleton together while allowing movement. Joints are called articulations; they
are points of contact between bones. Ligaments and tendons are connective
tissues that stabilize many joints.
5.5a Joints vary from immovable to freely movable
Joints are classified by degree of movement into
three classifications:
1.
Immovable
2.
Slightly
movable
3.
Freely
movable
There are three types of joints:
1.
Fibrous
2.
Cartilaginous
3.
Synovial
Fibrous joints are immovable. These immovable
joints firmly connect the bones that protect and stabilize the skull and brain.
At birth, fibrous joints are the flat bones in a baby’s skull that is separated
by large spaces filled with fibrous connective tissue (soft spots). These soft
spots or fontanels enable the baby’s
head to change shape, so that it can squeeze safely through the mother’s pelvic
opening during birth. As the baby matures, the fibrous joints harden and
gradually become thin lines between skull bones.
Cartilaginous joints are slightly moveable allowing for some degree in motion. Cartilaginous joints connect the vertebrae in the backbone and those that attach the lower ribs to the sternum via hyaline cartilage.
Synovial joints are freely moveable in which the bones are separated by a thin fluid-filled cavity. The two bones of a synovial joint are fastened together and stabilized by ligaments. The interior of the cavity is lined with a synovial membrane, which secretes synovial fluid to lubricate and cushion the joint. To reduce friction the articulating surfaces of the two bones are covered with hyaline cartilage, a tough but smooth layer of cartilage. Together the synovial membrane and the surrounding hyaline cartilage constitute the joint capsule.
Different types of synovial joints permit different kinds of movements:
1.
Hinge
joint (elbow/knee)
2.
Ball-and-Socket
joint (shoulder and hip)
The hinge joint allows movement only in one
direction.
The ball and socket joint permits movement in all directions such as in between the upper leg and hipbones and in between the upper arm and the pectoral girdle.
There are different types of movements made possible
by hinge and ball-and-socket joints (Oellers, Online Presentation, 2012):
Retrieved April
10, 2012.
·
Abduction is the movement
of a limb away from the body’s midline
·
Adduction is the movement
of a limb toward the body’s midline
·
Rotation is movement
around its own axis
·
Circumductions is movement of a
limb that describes a cone
·
Flexion decreases the
angle of a joint
·
Extension increases the
angle of a joint
·
Hyperextension is the
extension of a limb beyond its limit
·
Supination is the rotation
of the forearm so that the palm faces forwards
·
Pronation is the rotation
of the forearm so that the palm faces backwards
REFERENCES
Johnson, M. D. (2012, 2010, 2008).
Human Biology: concepts and current issues, sixth edition. Pearson Education,
inc.; Benjamin Cummings.
Oellers, J. (n.d). Online
Presentation: Ch. 5 The Skeletal System. Retrieved April 10, 2012, from http://lblackboard.yc.edu/webapps/portal/frameset.jsp?tab_tab_group_id=_2_1&url=%2Fwebapps%2Fblackboard%2Fexecute%2Flauncher%3Dcourse%26id%3D_43466_1
Science News (April 15, 2012). New
Genetic Regions linked to Bone-weakening Diseases and Fractures. Retrieved
April 10, 2012 from
Ch. 6 The
Muscular System
Table of Contents
6.1 Muscles produce movement or generate tension
a. The fundamental activity of
muscle is contraction
b. Skeletal muscles cause bones to
move
c. A muscle is composed of many
muscle cells
d. The contractile unit is a
sarcomere
6.2 Individual muscle cells contract and relax
a. Nerves activate skeletal muscles
b. Activation releases calcium
c. Calcium initiates the sliding
filament mechanism
d. When nerve activation ends,
contraction ends
e. Muscles require energy to
contract and to relax
6.4 Cardiac and smooth muscles have special features
a. How cardiac and smooth muscles
are activated
b. Speed and sustainability of
contraction
c. Arrangement of myosin and actin
filaments
6.1 Muscles
produce movement or generate tension
The body has three types of muscle (Johnson 2012):
Smooth Muscle
http://www.sciencelearn.org.nz/Contexts/Sporting-Edge/Science-Ideas-and-Concepts/Muscle-structure-muscle-under-the-microscope,
Retrieved April 9, 2012.
1.
Skeletal
2.
Cardiac
3.
Smooth
The muscles main
function is to produce movement or generate tension (Oellers, Online Presentation,
2012). The principle function of a muscle is to contract, which is the
shortening distance between bones.
Skeletal muscle contraction is initiated by
nerve activity only. Contraction requires energy that ultimately comes from
stored carbohydrates or fats. Men consist of 40% skeletal muscle while women
have 32% skeletal muscle (Johnson 2012). Skeletal muscles have many duties but
a few examples are that skeletal muscles help control the focus of our eye and
are responsible for us shivering when we are cold.
Some muscle
movements are voluntary meaning we have control over their movement. Other
muscle movement is involuntary for example your heart beat.
Muscles must
generate heat in order to maintain homeostasis of our body temperature. Our
body temperature is usually higher than our surroundings unless it is chili
outside and then shivering occurs so that the muscles will contract and relax
to generate heat.
6.1a The
fundamental activity of muscle is contraction
The three types of muscle cells (skeletal, smooth
and cardiac) have similar features such as (Johnson 2012):
·
Muscle
cells contract in response to chemical or electrical signals from other organ
systems
·
All
muscles contract (shorten) and relax
6.1b Skeletal
muscles cause bones to move
Skeletal muscles
attach to the skeleton via tendons or attach to other muscles or to the skin
and give us strength and mobility. A good example of skeletal muscles in action
is allowing us to pick up tiny objects or any object.
The muscles are
organized into pairs that are controlled by nerve activity only.
Muscle groups
either work together which is called synergistic
for example the pectorals and the triceps. These two muscles work together when
doing a pushup, the triceps straightens the arm and the pectorals stabilize the
upper body. Muscle groups that work against each other called antagonistic for instance, the forearm
bends, when the biceps contracts and the triceps relax.
Each individual
muscle produces a specific movement of one bone relative to another.
http://www2.sluh.org/bioweb/bi100/tutorials/musclephysiology/origin-insertion.png, Retrieved
April 9, 2012.
Skeletal muscles
consist of an origin and insertion, which are the points of attachment to a
muscle. The origin is the point of
attachment of a muscle to the stationary bone, for example the scapula (Oellers,
Online Presentation, 2012). The insertion
is the point of attachment to the moveable bone, for example the biceps are
attached via tendon to the insertion point and is attached to the radius across
the joint (Oellers, Online Presentation, 2012). When a muscle contracts, the
insertion is pulled toward the origin, which is closer to the midline of the
body.
6.1c A muscle is
composed of many muscle cells
A single or
whole muscle is a group of individual muscle cells that all have the same origin
and insertion with the same functions (Johnson 2012).
A muscle is
arranged in bundles called fascicles
each composed of many muscle cells and each surrounded by connective tissue (fascia). The fascia join together to
become the tendon that attaches muscle to bone. Each fascicle contains a few
dozen to 1000 of individual muscle cells or muscle fibers. Several layers of
fascia cover the outer surface of the muscle. Individual muscle cells or muscle
fibers are long and tube shaped (Oellers, Online Presentation, 2012). Each
muscle contains more than one nucleus and contains myofibrils, which are long cylindrical structures arranged parallel
and consume the entire interior of a cell (Johnson 2012). Myofibrils contain
contractile proteins, actin and myosin (Oellers Online Presentation 2012).
Sacromeres is the contractile unit in a myofibril.
Myofibril is composed of sacromeres joined end to end at the Z-line. Z-lines are attachment points for
sacromeres (Oellers, online Presentation, 2012). Sacromeres contain thin
filaments of actin that attach to the Z-lines and thicker filaments of myosin
that span the gap between actin molecules.
6.2 Individual
muscle cells contract and relax
During a muscle contraction,
each sacromere shortens a little.
Contraction is
what bridges the thick myosin and thin actin filaments (Oellers, Online
Presentation, 2012).
Four things contribute to a skeletal muscle cell to
contract and relax
(Johnson 2012):
1.
Must
be activated by a nerve
2.
Nerve
activation increases calcium
3.
Calcium
must be present for the muscles to contract
4.
When
a muscle cell is no longer stimulated by a nerve, contraction ends
6.2a Nerves
activate skeletal muscles
Motor neurons are nerves that stimulate skeletal
muscle cells to contract. Motor neurons secrete a chemical called acetylcholine (ACH), which activates
the cells to contract. The gap between the motor neurons and skeletal muscle
cell is called the neuromuscular
junction. For contraction to happen an electrical impulse must be able to
bridge the gap. When an electrical impulse reaches the neuromuscular junction,
acetylcholine releases. ACH then binds to receptor sites on the muscle cell
membrane and is carried to the cell’s interior by T tubules. The function of
the T tubules is to get the
electrical impulse to all parts of the cell as quickly as possible (Johnson
2012). Myosin crosses over the bridge and draws the actin molecules closer
together.
Science Daily
April 11, 2012 wrote an article about a childhood disorder called spinal
muscular atrophy (SMA) has been linked to an abnormally low level of a protein
in certain nerve cells. SMA causes a child’s motor neurons to produce
insufficient amounts of survival motor neuron protein (SMN). This causes the
motor neurons to die leading to muscle weakness and the inability to move.
There is no cure, but medicines and physical therapy help treat symptoms.
6.2b Activation
releases calcium
The electrical
impulse caused by the ACH (Acetylcholine) triggers the release of ionic calcium
(Ca2+) from the sacroplasmic reticulum
(SR), which stores the ionic calcium. The calcium then diffuses into the
cells’ cytoplasm and the myosin-binding site is exposed. Myosin heads form
cross-bridges with actin and the actin filaments are pulled toward the center
of the sarcomere. Contraction then commences.
http://en.wikipedia.org/wiki/Sliding_filament_model, Retrieved April 9, 2012.
Muscles contract
when sarcomeres shorten and they shorten when the actin and myosin filaments
slid past each other, known as the sliding
filament mechanism of contraction (Johnson 2012). During contraction, the
myosin (resembles a golf club) heads form a bridge with actin and then bend
pulling the actin filaments toward the center of the sacromere.
In a relaxed
state, nerve activation and contraction ends, the myosin heads do not make
contact with actin. Calcium is pumped back into the sacroplasmic reticulum and
calcium is also removed from the troponin therefore covering the myosin binding
site. Muscles can relax because a protein molecule closely associated with the
actin filaments called troponin and
tropomyosin interfere with the myosin binding sites on the actin molecule
in the absence of calcium. No calcium equals no cross-bridges, therefore
contraction cannot happen.
When an
electrical impulse happens, calcium is released from the sarcoplasmic reticulum
and binds to troponin. This results in a shift of position, exposes the myosin
binding sites, and permits the bridges pulling the actin filaments toward the
center of the sacromere from each end.
6.2d When nerve
activation ends, contraction ends
Relaxation of a
muscle cell occurs when nerve activity ends.
ATP is required
for contraction and relaxation (Oellers, Online Presentation, 2012).
ATP is needed to
transport the calcium used for muscle contraction back to the SR for storage.
As calcium decreases in the myofibril, the troponin-tropomyosin protein shifts
back to its original position blocking the bridges to actin.
The interference
of nerve cells can disrupt muscle function. Myasthenia gravis is a disorder which the body’s immune system
attacks and destroys ACH receptors on the cell membrane of muscle cells. Resulting
in muscles not being able to contract. This disorder can cause droopy eyelids
and double vision.
6.2e Muscles
require energy to contract and relax
Muscle
contraction requires ATP. In the presence of calcium, myosin splits ATP into
ADP releasing energy to do work. The energy is used to energize the myosin so
that it can form a bridge to the actin. As long as calcium is present, the cycle
of ATP breakdown repeats. The result is a shortening of the sacromere. After contraction,
ATP is used to transport calcium back into the SR so that relaxation can occur.
For relaxation to happen, an intact molecule of ATP must bind to myosin so that
it can detach from actin. Muscle cells store only enough ATP for ten seconds
worth (Johnson 2012).
Once this energy is used up, cells must
replenish ATP by (Oellers, Online Presentation, 2012):
·
Creatine
Phosphate
·
Stored
Glycogen
·
Aerobic
Metabolism of Glucose, fatty acids and other high energy molecules
Creatine phosphate is a high-energy molecule with
an attached phosphate group that transfers a phosphate group and energy to ADP
and can create a new ATP molecule quickly. If ATP is not needed to power muscle
contraction the excess ATP can be used to build a fresh supply of creatine
phosphate, which is stored until needed. The combination of previous ATP plus
stored creatine phosphate produces enough energy for thirty to forty seconds
(Johnson 2012). Beyond that, muscles rely on stored glycogen (a complex sugar).
Glucose molecules are removed from glycogen and
energy is used to create ATP. This breakdown of glucose happens without oxygen
called anaerobic metabolism (Johnson 2012).
The most
efficient long-term source of energy is the aerobic (takes place in the mitochondria and requires oxygen) metabolism of glucose in the blood,
fatty acids derived from stored fat in fat cells and lactic acid (caused the burning sensation) (Johnson 2012).
After exercising,
you continue to breathe heavily for a period of time. These deep breaths help
reverse your body’s oxygen debt, because your muscles used more ATP early on
than was provided by aerobic metabolism. The addition of ATP is provided by
anaerobic metabolism with the buildup of lactic acid. The ability of muscle
tissue to accumulate an oxygen debt and then repay it later allows muscles to
perform at a near-maximal rate even before aerobic metabolism has increased
(Johnson 2012).
Muscle fatigue is a decline in muscle
performance during exercise caused by insufficient energy to meet metabolic
demands due to depletion of ATP, creatine phosphate and glycogen stores within
the muscle.
6.4 Cardiac and
smooth muscles are activated
The cardiac muscle’s rhythmic contractions
of the heart pump blood throughout the body. Smooth muscles in the walls of the uterus propel the child through
the birth canal; they also push food through the digestive tract and transport
urine from the kidneys to the bladder.
Cardiac Muscle
Cardiac and
smooth muscles are involuntary muscles. We have no control over them. They can
contract without signals from the nerves, however; they both do respond to
nerve activity. All cardiac muscle cells establish their own cycle of
contraction and relaxation, those with the fastest rhythm are called pacemaker cells because they set the
pace for the rest of the cells to follow. Cardiac muscle cells are joined at
their blunt ends by intercalated discs;
they contain gap junctions that permit one cell to electrically stimulate the
next one.
Smooth muscle
cells are joined by gap junctions, which permit the cells to activate each
other so that the whole tissue contracts together. Cardiac and smooth muscle
cells can contract without signals from the nervous system; however, they both
respond to the nervous system. The effect of nerve activity may be either
inhibitory or stimulatory. Changes in both inhibitory and stimulatory nerve activity
to the heart are responsible for the increase in your heart rate when you
exercise.
6.4 b Speed and
sustainability of contraction
Skeletal muscle
is the fastest muscle to contract, next is the cardiac muscle, which is moderately
fast and then smooth muscle which contract very slow.
Cardiac muscles
have contraction and relaxation cycle’s so the muscle will not fatigue.
Smooth muscles
are partially contracted all the time. These muscles never fatigue because they
contract so slowly that their ATP usage is always less than its procuring
capability. Smooth muscles are the key player in the regulation of blood
pressure (Johnson 2012).

http://www.britannica.com/EBchecked/media/46939/The-structure-of-striated-muscle-Striated-muscle-tissue-such-as, Retrieved April 9, 2012.
Cardiac muscle has thick and thin filaments arranged in sarcomeres called striated muscle (Johnson 2012).
The thick and thin filaments in smooth muscle are arranged in bundles that attach at various angles to the cell membrane. When these filaments slide past each other, the points of attachment are pulled toward each other and the cell gets shorter and fatter. Since the filaments are arranged in bundles other than sacromeres, the muscle is smooth in appearance other than having the striated look.
REFERENCES
Johnson, M. D. (2012, 2010, 2008).
Human Biology: concepts and current issues, sixth edition. Pearson Education,
inc.; Benjamin Cummings.
Oellers, J. (n.d). Online
Presentation: Ch. 6 The Muscular System. Retrieved April 9, 2012, from http://lblackboard.yc.edu/webapps/portal/frameset.jsp?tab_tab_group_id=_2_1&url=%2Fwebapps%2Fblackboard%2Fexecute%2Flauncher%3Dcourse%26id%3D_43466_1
Science News (April 11, 2012). Possible
cause of movement defects in spinal muscular atrophy identification. Retrieved
April 12, 2012 from http://www.sciencedaily.com/releases/2012/04/120411102723.htm
Ch. 7 Blood
Table of Contents
7.1 The components and functions of blood
a. Plasma consists of water and
dissolved solutes
b. Red blood cells transport oxygen
and carbon dioxide
c. Hematocrit and hemoglobin reflect
oxygen-carrying capacity
d. All blood cells and platelets
originate from stem cells
e. RBCs have a short life span
f. RBC production is regulated by a
hormone
g. White blood cells defend the body
1. Granular leukocytes:
Neutrophils, eosinophils, and basophils
2. Agranular leukocytes:
Monocytes and lymphocytes
h. Platelets are essential for blood
clotting
7.2 Hemostasis: Stopping blood loss
a. Platelets stick together to seal
a ruptured vessel
b. A blood clot forms around the
platelet plug
7.3 Human blood types
a. ABO blood typing is based on A
and B antigens
b. Rh blood typing is based on Rh
factor
c. Blood typing and cross matching
ensure blood capability
7.1 The
components and functions of blood
The main human
blood types are types A, B, AB and O. Blood type is determined by proteins
called antigens on the surface of
red blood cells. The circulatory system consists of the heart, the blood
vessels and the blood that circulates through them (Johnson 2012). Blood is a
connective tissue consisting of specialized cells and cell fragments suspended
in a watery solution of molecules and ions (Johnson 2012).
There are three primary functions of blood (Oellers,
Online Presentation, 2012):
1.
Transporting
of nutrients, waste and hormones. Blood transports oxygen from the lungs,
nutrients from the digestive system, and hormones from the endocrine glands and
waste from body tissues to the organs for proper disposal.
2.
Regulation
of body temperature, water volume in the body and pH of body fluids.
3.
Defense
against infections and excessive bleeding by clotting.
These functions
are crucial for maintaining homeostasis.
Components of blood fall into two major categories (Oellers Online
Presentation 2012):
1.
Liquid
Component: 55% Plasma (water,
electrolytes, proteins, hormones, gases, nutrients and wastes.
2.
45%
Cellular component or formed
elements such as red blood cells, white blood cells and platelets.
7.1a Plasma consists of water and dissolved solutes
90% of plasma is water and the rest is dissolved proteins, hormones and other small molecules.
Plasma proteins are the large group of solutes in plasma that include albumins, globulins and clotting proteins.
Albumins is manufactured in the liver and
maintains the water balance between blood and interstitial fluid while
assisting some molecules and drugs in their transport in blood (Johnson 2012).
Globulin (alpha, beta and gamma) proteins
transport various substances in the blood.
Beta globulins bind to lipid (fat) molecules creating a lipoprotein. Lipoproteins can be low-density lipoproteins (LDL) called the “bad cholesterol” that causes high blood pressure and increases the risk of cardiovascular disease and high-density lipoproteins (HDL). High levels of HDLs often indicate a lower risk of cardiovascular disease (Johnson 2012).
Clotting proteins prevents the excessive loss of
blood by blood clotting.
Plasma transports other molecules including ions (electrolytes), hormones, nutrients, waste products and gases.
Electrolytes (Na/Potassium) control cell functions and cell volume.
Hormones
transport information throughout the body.
Nutrients are
absorbed from the digestive tract or produced by cells’ metabolic reactions.
Waste produced in plasma includes:
·
carbon
dioxide
·
urea
·
lactic
acid.
Gases dissolved
in plasma are oxygen, which is necessary for metabolism and carbon dioxide.
Waste is a product of metabolism.
7.1b Red blood cells transport oxygen and carbon dioxide
www.adam.com, retrieved April
8, 2012.
The main
function of red blood cells (RBCs)
is to carry oxygen and carbon dioxide. They are small, flattened,
doughnut-shaped disks with thin concave centers and thick edges (Johnson 2012).
Their structure helps RBC’s to be flexible allowing them to squeeze through
tiny blood vessels. RBCs’ have no nucleus and contain no organelles. They are
fluid-filling bags of plasma membrane and molecules of an oxygen-binding
protein called hemoglobin (oxygen-carrying compound in RBCs), which consists of
four polypeptide chains folded together each with a heme group containing a
single iron atom. There are approximately 300 million of these molecules in
every red blood cell. The iron atom forms bonds with oxygen molecules. A RBC
can carry up to 1.2 billion molecules of oxygen.
Several factors influence the binding of hemoglobin to oxygen:
·
The
concentration of oxygen must be high
·
The pH neutral. The lungs are a great place
for this.
Oxygen
is diffused into the blood plasma and then into RBCs, where it attaches to the
iron atoms in the hemoglobin.
A
picture of hemoglobin. The green, yellow, blue, and gray colors make up
the four-polypeptide subunits of hemoglobin. Each subunit has its own heme
group (shown in red.) The heme group is where the oxygen binds.
http://www.psc.edu/science/Ho/Ho.html, Retrieved
April 8, 2012.
Hemoglobin that has given up its oxygen is called deoxyhemoglobin and is a dark purple color. Hemoglobin also transports carbon dioxide (waste product of cellular metabolism).
7.1c Hematocrit
and hemoglobin reflect oxygen-carrying capacity
Hematocrit is the percent of blood that consist of RBCs’. Normal hematocrit is 43 to 49 % for men and 37-43% for women (Johnson 2012). A low hematocrit may signal anemia (inadequate supply of hemoglobin in the RBCs) or other disorders of RBC production. A high hematocrit can signal polycythemia, a disorder of the bone marrow by an over production of RBCs.
7.1d All blood cells and platelets originate from stem cells
All blood cells
and platelets originate from bones called stem
cells that are constantly dividing in order to create immature blood cells
(Johnson 2012). These blood cells develop into platelets and various types of
mature red and white blood cells. Even stem cells from the pelvic bone may help
hearts beat stronger. Science Daily (April 11, 2012) states in their article
that researchers are using stem cells from pelvic bone marrow to restore tissue
and improve heart function after muscle damage and heart attacks. By infusing
certain stem cells into the area of the heart muscle that has been damaged from
a heart attack, tissue can be preserved and heart function restored.
7.1e RBCs have a
short life span
http://www.funsci.com/fun3_en/blood/blood.htm#contents, Retrieved
April 8, 2012.
Some stem cells
develop into immature cells called erythroblasts.
They fill with hemoglobin and develop into mature RBCs within a week. They
cannot reproduce because they have no nucleus or organelles and die out
quickly.
RBCs originate
from stem cells in bone marrow and have a short life span that is approximately
120 days (Oellers, Online Presentation, 2012). Within that time they make
approximately 3000 round trips carrying oxygen from the lungs to the tissues
and carbon dioxide from the tissues back to the lungs (Johnson 2012). Erythropoietin is a hormone that
contains no nucleus and controls production of RBCs. To keep the hematocrit
constant RBCs must be produced at a rate of more than 2 million per second
(Johnson 2012).
Old and damaged
RBCs are removed from the circulating blood and destroyed in the liver and
spleen by large cells called macrophages
by a process call phagocytosis. Macrophages are derived from monocytes the largest of the white
blood cells (WBCs).
When the hemoglobin in RBCs are broken down in the liver, bilirubin mixes with bile and is secreted during digestion, which passes into the intestines. This pigment contributes to the colors of the urine and feces. Bilirubin is a yellowish pigment in the liver that the heme groups minus the iron are converted to during the breakdown of RBCs.
7.1f RBC
production is regulated by a hormone
The hormone Erythropoietin regulates RBC production
(Oellers, Online Presentation, 2012). The regulation of RBC production is a
negative feedback control loop that maintains homeostasis. The number of RBCs
are not regulated, just their ability to transport oxygen. The cells in the
kidneys monitor the availability of oxygen (Oellers, Online Presentation,
2012). If the levels fall, the cells in the kidneys secrete erythropoietin,
which is transported in the blood to the red bone marrow where it stimulates
stem cells to produce more RBCs (Oellers, Online Presentation, 2012). People
who suffer from a kidney disease do not produce enough erythropoietin to
regulate RBC production properly. Erythropoietin is now available commercially
for these individuals (Johnson 2012).
Blood doping is injecting erythropoietin (Johnson
2012). It is a practice used by some athletes to increase their blood-oxygen
carrying capacity.
7.1g White blood
cells defend the body
Approximately
one percent of whole blood consists of white blood cells (WBCs) or leukocytes (Johnson 2012). WBCs are
larger than RBCs. They contain a nucleus but no hemoglobin. There is one WBC
for every 700 RBCs (Johnson 2012). WBCs originate from stem cells in the red
bone marrow.
The function of
WBCs is to protect from infection and regulate inflammatory reaction (Oellers, Online
Presentation, 2012).
There are two categories of WBCs (Oellers,
Online Presentation, 2012):
1.
Granular
leukocytes
(granulocytes)
2.
Agranular
leukocytes
(agranulocytes)
Both types
contain granules (vesicles) in their
cytoplasm that is filled with proteins and enzymes to assist in their defensive
work.
WBCs have a
short life span and many granular leukocytes die within a few hours to nine
days due to injuries while fighting microorganisms. WBCs are constantly removed
from the blood by the liver and spleen.
WBCs increase
when viruses, bacteria, etc threaten the body. When activated by either tissue
injury or microbes each type of WBC produces chemical that stimulates the
production of new WBCs from the bone marrow.
7.1 g, 1
Granular leukocytes: Neutrophils, eosinophils, and basophils
http://www.webmd.com/heart/anatomy-picture-of-blood, Retrieved April 8, 2012.
Neutrophils are the first WBC to combat infection
by engulfing foreign cells and are 60% of circulating WBCs (Oellers, Online
Presentation, 2012).
Eosinophils are two to four percent of circulating
WBCs and have two functions (Johnson
2012):
1.
Defend
the body against large parasites, such as worms, by forming clusters of
eosinophils that surround each parasite and bombard it with digestive enzymes.
2.
They
also release chemicals that moderate the severity of allergic reactions.
Basophils is .5% of circulating WBCs (Oellers,
Online Presentation, 2012). When body tissue are injured basophils secrete histamine (a chemical that initiates
the inflammatory response) causing adjacent blood vessels to release blood plasma
into the injured area. The plasma brings in nutrients, various cells, chemicals
to begin tissue repair.
7.1g, 2 Agranular
leukocytes: Monocytes and lymphocytes
Monocytes is five percent of the circulating WBCs
(Oellers, Online Presentation, 2012). Monocytes are the largest WBC. They
filter out the bloodstream and live in body tissues where they differentiate
into macrophages (removes RBCs) and engulf invaders. They also stimulate
lymphocytes to defend the body.

A picture of a
Lymphocyte
http://en.wikipedia.org/wiki/Lymphocyte, Retrieved
April 8, 2012.
Lymphocytes consist of thirty percent of circulation WBCs (Oellers, Online Presentation, 2012). Lymphocytes are found in the blood stream, tonsils, spleen, lymph nodes and thymus gland.
They can be classified into two types (Johnson 2012):
1.
B-lymphocytes (B
cells)
give rise to plasma cells that produce antibodies that defend against
microorganisms and invaders.
2.
T lymphocytes (T
cells)
target and destroy bacteria, viruses and cancer cells.
7.1h Platelets
are essential for blood clotting
Less than one
percent of whole blood consist of platelets (Johnson 2012). Platelets are small cell fragments
derived from megakaryocytic (large
cells derived from stem cells in bone marrow) that play an important role in
homeostasis (Oellers, Online Presentation, 2012).
Platelets are
not living cells that last approximately five to nine days in the circulation
(Johnson 2012). Platelets participate in blood clotting when a blood vessel is
injured. During the repair process, platelets release proteins that promote
blood vessel growth and repair.
7.2 Hemostasis:
Stopping blood loss

A picture of the process of Hemostasis
http://www.google.com/search?hl=en&safe=active&biw=1243&bih=904&gbv=2&tbm=isch&sa=1&q=hemostasis&aq=f&aqi=g10&aql=&oq=#q=hemostasis&hl=en&safe=active&gbv=2&tbm=isch&bav=on.2,or.r_gc.r_pw.r_qf.,cf.osb&fp=1&biw=1680&bih=882, Retrieved April 8, 2012.
Hemostasis has three stages (Oellers, Online Presentation, 2012):
1.
Vascular
spasm or intense contraction of blood vessels to decrease blood flow.
2.
Platelet
plug formation- the sealing of a ruptured blood vessel
3.
Coagulation
or blood clotting
7.2a Vascular
spasms constrict blood vessels to reduce blood flow
When a blood
vessel is damaged, it contracts to decrease blood flow. Depending on the vessel
size, can determine the reduction of blood flow speed. Small vessels contract
and press the inner walls together and may stop the bleeding entirely.
7.2b Platelets
stick together to seal a ruptured vessel
Platelets under
normal conditions circulate freely; however, when a blood vessel is damaged
platelets swell and develop spiky extensions. Platelets then begin to clump
together resulting in a platelet plug that seals the injured area.
7.2c A blood
clot forms around the platelet plug
The three stages
in hemostasis (vascular spasm, platelet plug formation and blood clotting) is
where the blood changes from a liquid to a gel creating a blood clot.
This involves a series of chemical reactions of
three important clotting factors:
1.
Prothrombin
activator
2.
Thrombin
3.
Fibrinogen
Prothrombin activator is released
when there is damage to a blood vessel. This activates the conversion of
prothrombin (a plasma protein) into an enzyme called thrombin. This requires
calcium ions (Ca2+). Thrombin then
facilitates the conversion of a soluble plasma protein fibrinogen into long insoluble threads of a protein called fibrin. The fibrin threads wind around
the platelet plug that traps and holds platelet blood cells and various
molecules against the opening. This results in an initial clot that decreases
the flow of blood. Platelets in the clot start to contract, tightening the clot
and pulling the vessel walls together. The blood clotting formation takes less
than an hour to form (Johnson 2012).
A blood clotting
disorder can be deadly. Hemophilia is
a deficiency of one or more blood clotting factors (Johnson 2012). When a
vessel is breached, blood clots slowly or not at all. This is due to factor
VIII (a protein) missing (Johnson 2012).
7.3 Human blood
types
Blood transfusion is putting foreign blood
directly into the bloodstream of another person (Johnson 2012). Success depends
largely on blood type, which is based on the ABO blood group system.
Blood typing deals with antigens (surface markers on RBCs) and antibodies (immune system protein, directed against antigens)
(Oellers, Online Presentation, 2012).
Blood must be
compatible when having a blood transfusion in order for our WBCs to not
activate because of the blood not being compatible. The body recognizes these
cells to be foreign cells that carry different surface proteins. The WBCs
recognize these foreign cells as “nonself”.
An antigen is a nonself cell protein that
stimulates the immune system. As part of the WBCs defense, the immune system
produces an opposing protein called an antibody. Produced by lymphocytes antibodies belong to plasma proteins
called gamma globulins (Johnson 2012). These antibodies attack the antigens,
however; only a specific antibody can attack a specific antigen. Antibodies
float freely in the blood and lymph until they encounter an invader with the
matching antigen.
7.3a ABO blood
typing is based on A and B antigens
RBCs are
classified by the ABO blood group system.
http://www.google.com/search?hl=en&safe=active&biw=1243&bih=904&gbv=2&tbm=isch&sa=1&q=hemostasis&aq=f&aqi=g10&aql=&oq=#q=hemostasis&hl=en&safe=active&gbv=2&tbm=isch&bav=on.2,or.r_gc.r_pw.r_qf.,cf.osb&fp=1&biw=1680&bih=882, Retrieved April 8, 2012.
There are four types:
1.
Type
A
2.
Type
B
3.
Type
AB
4.
Type
O
Type A blood has A antigens and makes B antibodies, type B blood has B antigens and makes A
antibodies, type AB blood make both A and B antigens and produces
neither A or B antibodies and type O
blood has neither A or B antigens and produces A and B antibodies.
All individuals
have circulating antibodies that fight against surface antigens different from
their own. Antibodies appear early in life and attack RBCs with foreign
antigens, damaging them and causing them to clump together (agglutinate). This can result in blood
vessels becoming blocked, organ damage or death if agglutination is extreme
(Johnson 2012).
Any adverse
effect of a blood transfusion is called a transfusion
reaction (Johnson 2012). If you have type A blood you are restricted to
receiving transfusions of type A or type O blood because neither of them has a
foreign (type B) antigen and vice versa. People with type AB blood can receive
transfusions from A, B, O, but not from other AB individuals. People with AB
blood can donate only to other type AB people. Type O people can give blood to
people of A, B or AB type, but they can receive blood only from Type O people.
The antibodies of the recipient generally cause the transfusion reaction.
7.3b Rh blood
typing is based on Rh factor
Rh factor is a RBC surface antigen that is important in blood transfusion. People either carry Rh on their RBCs or do not. People who are Rh-negative meaning they are not equipped with the Rh antigen, their immune system will respond to any foreign Rh antigen by making antibodies against it. Being Rh negative is a concern for pregnant women especially if they become pregnant by an Rh-positive man. If the fetus is Rh positive, its blood cells can leak into the mother’s blood and cause the mother to start producing anti-Rh antibodies. These antibodies can cross the placenta and attack the fetus’ RBCs. This can cause the fetus to have mental retardation or even death (Johnson 2012). To prevent this and Rh negative mother carrying an Rh positive child the mother is given an injection of anti-Rh antibodies at 28 weeks (Johnson 2012). This injection destroys any of the child’s RBCs that may have entered the mother’s circulation during childbirth, before her immune system has time to react.
Blood typing has several purposes. Here are a few (Johnson 2012):
·
Used
in criminal investigations to compare the blood of victims and perpetrators
·
DNA
tests to determine paternity
7.3c Blood
typing and cross matching ensure blood compatibility
Blood typing involves determining your ABO type and
the presence or absence of the Rh factor. For example, B positive means that you
have type B blood and are positive for the Rh factor, (O-) means you have type
O blood and negative for the Rh factor.
Cross matching involves mixing small samples of donor blood with recipient plasma and recipient blood with donor plasma and examining both combinations for agglutination to be safe.
REFERENCES
Johnson, M. D. (2012, 2010, 2008).
Human Biology: concepts and current issues, sixth edition. Pearson Education,
inc.; Benjamin Cummings.
Oellers, J. (n.d). Online
Presentation: Ch. 7 Blood. Retrieved April 8, 2012, from http://lblackboard.yc.edu/webapps/portal/frameset.jsp?tab_tab_group_id=_2_1&url=%2Fwebapps%2Fblackboard%2Fexecute%2Flauncher%3Dcourse%26id%3D_43466_1
Science News (April 11, 2012). Stem
cells from pelvic bone may preserve heart function. Retrieved April 12, 2012
from http://www.sciencedaily.com/releases/2012/04/120411102434.htm
Ch.
8 Heart and Blood Vessels
Table of
Contents
8.1 Blood vessels transport blood
a. Arteries transport blood away
from the heart
b. Arterioles and precapillary
sphincters regulate
c. Capillaries: Where blood
exchanges substances with tissues
d. Lymphatic system helps maintain
blood volume
e. Veins return blood to the heart
1. Skeletal muscles
squeeze veins
2. One-way valves permit
only one-way blood flow
3. Pressures associated
with breathing push blood toward the heart
8.2 The heart pumps blood through the vessels
a. The heart is mostly muscle
b. The heart has four chambers and
four valves
c. The pulmonary circuit provides
for gas exchange
d. The systemic circuit serves the
rest of the body
8.1
Blood vessels transport blood
The
structure of blood vessels reflects their function. Thick-walled arteries and arterioles transport blood to the tissues under high pressure; capillaries allow fluid exchange
between blood and interstitial fluid; large thin-walled veins store most of the
blood and return it to the heart (Johnson 2012). High fat diets can damage our
arteries reducing the amount of blood they transport to the heart. Science
Daily (April 3, 2012) state that high fat diets cause damage to blood vessels
and can cause high blood pressure. Researchers found that only after six weeks
of high fat feeding to mice that their structural and mechanical properties of
small arteries were rapidly altered. This can play a role in hypertension which
puts a strain on the heart and can lead to cardiovascular heart disease.
The
heart is a pump that is constructed entirely of living cells and cellular
materials. The heart and blood vessels are known as the cardiovascular system. The heart provides the power to move the
blood and the vascular system transports the blood to body parts. It is
essential to maintaining homeostasis.
Blood vessels transports
blood to all parts of the body.
1.
Blood rich in carbon
dioxide is pumped from the heart into the lungs through the pulmonary
arteries. (Arteries are blood vessels carrying blood away from the heart;
veins are blood vessels carrying blood to the heart.)
2.
In the lungs, CO2
in the blood is exchanged for O2.
3.
The oxygen-rich blood
is carried back to the heart through the pulmonary veins.
|
4.
This oxygen-rich blood
is then pumped from the heart to the many tissues and organs of the body,
through the systemic arteries.
5.
In the tissues, the arteries
narrow to tiny capillaries. Here, O2 in the blood is exchanged for
CO2.
6.
The capillaries widen
into the systemic veins, which carry the carbon-dioxide-rich blood back to
the heart.
|
http://www.chemistry.wustl.edu/~courses/genchem/Tutorials/Hemoglobin/effect.htm, Retrieved April 13, 2012.
Three types of
Blood vessels transport blood (Oellers, Online Presentation, 2012):
1.
Arteries contain thick
walls that carry blood away from the heart to body tissues under high pressure.
2.
Capillaries are microscopic
and exchange solutes and water with cells of the body.
3.
Veins contain thin
walls that store blood and return deoxygenated blood back to the heart.
8.1a Arteries transport blood away from the heart
Blood leaves the
heart and enters the arteries where the blood is transported throughout the
body. Arteries have thick walls ranging from medium to large size
enabling them to withstand the high pressure generated by the heart. Arteries
resemble the roots of trees; they branch out and out and the further, they go
the smaller in diameter the arteries become.
Arteries have
the ability to stretch under pressure so that they can store the blood that is
pumped into them with each beat of the heart and then provide it to the
capillaries at high pressure. The elastic recoil of arteries maintains the
blood pressure between heartbeats (Johnson 2012).
The structure of the artery vessel’s wall has three
layers as follows:
(Johnson 2012):
http://www.picsearch.com/index.cgi?q=picture+of+the+layers+of+arteries&width=1663, Retrieved
April 13, 2012.
·
The
thin innermost layer is the endothelium.
This layer is flat and is the squamous epithelial cells. It is the
continuation of the lining of the heart. The exterior of these cells are smooth
due to the cells being compact. This keeps friction to a minimum and promotes
smooth blood flow.
·
The
second layer is composed of smooth
muscle that is interwoven with elastic connective tissue. This is the thickest
layer of most arteries. When this layer contracts because of the smooth muscle,
the artery stiffens and helps resist the high pressure caused by the heart, but
it does not construct the artery to alter blood flow. The elastic tissue
interwoven into the smooth muscle allows the artery to stretch to accommodate
the blood that enters with each heartbeat.
·
The
outer layer is made of tough supportive connective
tissue that consists primarily of collagen. This layer anchors vessels to
surrounding tissues and helps protect them from injury.
Arteries
can easily sustain injury because of the high pressure created by the beating
of the heart. If the inner layer becomes damaged then blood can seep through
the injured area and separate the outer layers causing an aneurysm. Aneurysms cause the smooth muscle and endothelial layer (inner layer) to
bulge inward as they develop, narrowing the lumen or interior of the vessel to reduce blood flow to an organ or
region of the body. Aneurysms can cause severe chest pain or they can be
symptomless until they rupture causing massive internal bleeding that often
results in death.
Aneurysms
take years to develop and if detected can be repaired surgically. A stethoscope
can detect them. Doctors use a stethoscope to listen to the flow of blood and
can determine if an aneurysm has developed by this technique. A computerized
tomography (CT) scan can also locate aneurysms before they rupture.
8.1b
Arterioles and precapillary sphincters regulate blood flow
http://www.picsearch.com/imageDetail.cgi?id=-uy3_AuMBtSVuGvEJV9n8zrzCFoEM7L2rFmQ59GGTfY&width=1663&start=1&q=, Retrieved
April 13, 2012.
Arterioles are the smallest
arteries about the width of a piece of thread. By the time blood flows through
the arterioles, blood pressure has fallen considerable. Arterioles generally
lack the outer most layer of connective tissue and their smooth muscle layer is
not as thick.
Arterioles
store and transport blood as well as help regulate the amount of blood that
flows to each capillary. They accomplish this by contracting or relaxing the
smooth muscle layer, altering the diameter of the arteriole lumen.
Where
an arteriole joins a capillary there are bands of smooth muscles called precapillary sphincter. They serve as
gates that control blood flow into individual capillaries.
Vasodilatation increases blood
flow to capillaries, while vasoconstriction
(contraction of vascular smooth muscle) and precapillary sphincters reduce
arterioles diameter so reducing blood flow to the capillaries (Oellers, Online
Presentation, 2012).
Nerves,
hormones and conditions in the local environment of the arterioles and
precapillary sphincters can produce a wide variety of external and internal
factors of the vasoconstriction (Johnson 2012). For example, your fingers will
become pale if you go outside on a day when it is freezing. This happens
because the vasoconstriction produced by the nerves is narrowing your vessel
reducing heat loss from your body. Vice versa on a hot day, your skin will
appear flushed because the vasodilatation occurs to speed up heat loss and cool
you off.
8.1c
Capillaries: Where blood exchanges substances with tissues
Arterioles
connect to the smallest blood vessels called the capillaries.
Capillaries consist of thin
walls that allow red blood cells to pass through.
Networks
of capillaries are called capillary beds
and can be found in all regions of the body causing you to bleed no matter
where you are cut.
The
design of capillaries and their thin, porous walls allow blood to exchange
oxygen, carbon dioxide, nutrients, and waste products with tissue cells
(Johnson 2012). Capillary walls consist of a single layer of squamous
epithelial cells. Pores pierce this layer and the cells are separated by narrow
slits. The slits are large enough to allow the exchange of fluid and other
materials between blood and the fluid that surrounds every living cell (interstitial fluid), yet small enough
to retain red blood cells and most plasma proteins.
Capillaries
function as biological strains that permit selective exchange of substances
with the fluid surrounding the cell. Capillaries are the only blood vessels
that can exchange materials with the interstitial fluid.
8.1d
Lymphatic System helps maintain blood volume
There
is an imbalance between the amount of plasma fluid filtered by the capillaries
and the amount reabsorbed. This excess plasma fluid must be returned to the
cardiovascular system or all the plasma will end up in the interstitial fluid
(Johnson 2012).
http://www.web-books.com/eLibrary/Medicine/Physiology/Lymphatic/Lymphatic.htm, Retrieved
April 13, 2012.
The
lymphatic capillaries, which are a
system of blind-ended vessels that branch throughout our body tissues, pick up
the excess plasma fluid.
The
lymphatic system also picks up objects in the interstitial fluid that are too
large to diffuse into the capillaries which include lipid droplets absorbed
during digestion and invading organisms.
The
lymphatic capillaries transport the excess plasma fluid and large objects to
larger lymphatic vessels that will return the fluid to the veins near the
heart.
This
is how the lymphatic system maintains the proper volumes of blood and
interstitial fluid.
8.1e
Veins return blood to the heart
Veins
have three layers of tissue like arteries. Unlike arteries, veins consist of
much thinner walls of the outer two layers than arteries. Veins also have a
larger diameter lumen as well.
Veins
have thinner walls compared to arteries because there is not as much pressure
build up from the heart beating. As blood moves through the cardiovascular
system the blood pressure becomes lower and lower so by the time the blood
reaches the veins the pressure has decreased by a lot. The large diameter of
the veins allows them to stretch so that they can accommodate large volumes of
blood.
Veins
serve as a blood volume reservoir for the entire cardiovascular system. This is
approximately two-thirds of all the blood in your body (Johnson 2012). This
reservoir of blood allows your heart to continue beating when your body is
dehydrated keeping your blood pressure constant (Johnson 2012).
A
picture of varicose veins
http://www.medikkaclinic.com/Toronto_Varicose_Vein.html, Retrieved
April 13, 2012.
If
veins become dilated this can lead to varicose
veins which are permanently swollen veins that look bumpy from the pool of
blood. Veins become varicose when the leaflets of the valves no longer meet
properly and the valves do not work (Oellers, Online Presentation 2012). This
allows the blood to flow backwards and the veins enlarge. They are most common
in the feet and legs. Varicose veins can be treated by injecting a solution
that shrivels the vessels and makes them less visible. This will not affect the
blood flow because the undamaged adjacent veins will take over and return blood
to the heart.
Many parts assist the vein in returning blood to the heart (Oellers, Online Presentation, 2012):
1)
Contractions
of skeletal muscles
2)
One-way
valves inside the veins
3)
Pressure
changes associated with breathing
8.1e,
1 Skeletal muscles squeeze veins
Skeletal
muscles squeeze veins collapsing them and pushing blood back to the heart.
Moving around instead of standing still improves the return of blood to your
heart and prevents fluid buildup in your legs, which cause varicose veins.
8.1e,
2 One-way valves permit blood flow
One-way
valves permit blood flow only one way toward the heart. They open to permit
blood to move toward the heart and then close whenever the blood begins to flow
backwards. Together skeletal muscles and valves form the skeletal muscle pump
(Johnson 2012). Once blood has been pushed toward the heart by skeletal muscles
the blood cannot drain in the direction of gravity because of these one-way
valves. The opening and closing of these valves depend on the difference in
blood pressure on either side of the valve.
8.1e,
3 Pressures associated with breathing push blood toward the heart
Changes
in the chest (thoracic) and
abdominal cavities create a pressure change that aids in pushing blood toward
the heart (Johnson 2012). When we inhale, abdominal pressure increases and
squeezes abdominal veins. At the same time pressure within the thoracic cavity
decreases dilating thoracic veins. The result of these to actions create
pressure that pushes the blood toward the heart. This is sometimes called the respiratory pump.
8.2
The heart pumps blood through the vessels
A picture of a
human heart
http://www.picsearch.com/imageDetail.cgi?id=it9kiI6jHR5F0-G07gHNbV2xA90oKGHyt20facz4pAY&width=1663&start=1&q=picture
of a human heart, Retrieved April 13, 2012.
Your
heart is slightly larger than your fist and is cone shaped (Johnson 2012). The
heart is located in the chest cavity between the lungs and behind the sternum or
breastbone. The heart consists mostly of cardiac muscle that pumps ceaselessly
in a squeezing motion to propel blood through the blood vessels. The heart
pumps about 75 times every minute not including the increase in heart rate
(Johnson 2012). Under normal circumstances the heart’s rate of pumping is
controlled by the brain, but can also beat on its own without any instructions
from the brain.
8.2a
The heart is mostly muscle
The
heart is surrounded in a tough fibrous sac called the pericardium, which protects the heart, anchors it to surrounding
structures and prevents it from overfilling with blood (Oellers, Online Presentation
2012). The pericardial cavity
separates the pericardium from the heart. This cavity contains a film of
lubricating fluid that reduces friction and allows the heart and the
pericardium to glide smoothly against each other when the heart contracts (Johnson
2012).
The walls of the
heart consist of three layer (Oellers, Online Presentation 2012):
·
The
epicardium is the thin layer of the
epithelial and connective tissue
·
Myocardium is the thick
layer of cardiac muscle that contracts every time the heart beats squeezing the
chambers inside the heart and pushing blood outward into the arteries.
·
Endocardium
is the thin layer of the endothelial tissue that rests on a layer of connective
tissure.
Factors
that can lead to inflammation in or around the heart wall is infections,
cancer, injuries or complications from major surgery. Antibiotic and anti-inflammatory
drugs work well to combat against inflammation.
8.2b
The heart has 4 chambers and four valves
http://todaysseniorsnetwork.com/heart_health.htm, Retrieved April 13, 2012.
The
heart consists of four separate chambers (Oellers, Online Presentation):
·
Two
at the top are called the atria.
·
The two at the bottom are more muscular and
called the ventricles.
The septum is a muscular partition that
separates the right and left sides of the heart.
Blood
returning to the heart from the body’s tissues enters the heart at the right
atrium and passes through a valve into the right ventricle.
The
right ventricle is more muscular than the right atrium because it pumps blood
at pressure through a second valve and into the artery leading to the lungs.
Blood
returning from the lungs to the heart enters the left atrium and then passes
through a third valve into the left ventricle. The muscular left ventricle
pumps blood through a fourth valve into the body’s largest artery the aorta. From the aorta, blood travels through
the arteries and arterioles to the capillaries, venules and veins and then back
to the right atrium again (Johnson 2012).
The
left ventricle is more muscular than any of the heart’s four chambers because
this ventricle must generate pressures higher than the aortic blood pressure to
pump blood into the aorta.
The
right ventricle has thinner walls because the blood pressure in the arteries
leading to the lungs is about one-sixth that of the aorta.
Four
heart valves enforce the heart’s one-way flow pattern and prevents blood from
flowing backwards. The right and left atrioventricular
valves (AV) located between the atria and their adjacent ventricle prevents
blood from flowing back into the atria when the ventricle contract. The AV valves consist of thin connective
tissue flaps that project into the ventricles. These valves are supported by
strands of connective tissues called the chordae
tendineae that connect to muscular extensions of the ventricle walls called
papillary muscles (Johnson 2012). Together
these connective tissues prevent the valves from opening backwards into the
atria when the ventricle contract.
Two
semilunar valves (the pulmonary and
the aortic) prevent backflow into the ventricle from the main arteries leaving
the heart when the heart relaxes (Johnson 2012). Each semilunar valve consists
of three flaps.
8.2c
The pulmonary circuit provides for gas exchange
The
heart pumps blood through the lungs (the pulmonary
circuit) and throughout the rest of the body to all the cells (the systemic circuit) simultaneously. Each
circuit has its own set of blood vessels.
http://www.methuen.k12.ma.us/mnmelan/circulatory%20system%20notes47.htm, Retrieved
April 13, 2012.
When deoxygenated (Oxygen has been given
to tissue cells and taken up carbon dioxide) blood returns to the heart from
the veins it enters the right atrium.
1.
From
the right atrium, blood passes through the right atrioventricular valve into
the right ventricle.
2.
The
right ventricle pumps blood through the pulmonary semilunar valve into the pulmonary trunk (the main pulmonary
artery) leading to the lungs. The pulmonary trunk divides into the right and
left pulmonary arteries which supply the right and left lungs.
3.
At
the pulmonary capillaries, blood gives up carbon dioxide and receives a fresh
supply of oxygen from the air we inhale.
4.
The
freshly oxygenated blood flows into the pulmonary veins leading back to the
heart. It enters the left atrium and flows through the left atrioventricular
valve into the left ventricle.
The
deoxygenated blood in the right side of the heart never mixes with oxygenated
blood in the left. Deoxygenated blood leaving the right side of the heart must
pass through the pulmonary circuit (where it picks up oxygen) before it reaches
the left side of the heart.
Purpose of the
Circulatory System
(Oellers, Online Presentation 2012):
The
Circulatory System distributes
·
Heat
·
Water
·
Immune
System related cells
·
Carbon
Dioxide
·
Nutrients
·
Waste
When
blood enters the left ventricle, it begins the systemic circuit, which takes it to the rest of the body
The process of
the systemic circuit
(Oellers, Online Presentation, 2012):
1.
The
oxygenated blood travels from the left ventricle through the aortic semilunar
valve to the aorta.
2.
Through
the branching arteries and arterioles to the tissues.
3.
Through
the arterioles to capillaries.
4.
From
Capillaries into venules and veins.
5.
To
the vena cana and into the right atrium.
The
heart requires a great deal of oxygen and nutrients to fuel its own operations
so the heart has its own set of blood vessels called the coronary arteries. These arteries branch from the aorta just above
the aortic semilunar valve and encircle the heart’s surface. From there they
send branches inward to supply the myocardium. Cardiac veins collect the blood
from the capillaries in the heart muscle and channel it back to the right
atrium. The coronary arteries are small in diameter if they become blocked
serious health issues can result.
REFERENCES
Johnson, M. D. (2012, 2010, 2008).
Human Biology: concepts and current issues, sixth edition. Pearson Education,
inc.; Benjamin Cummings.
Oellers, J. (n.d). Online
Presentation: Ch. 8 Heart and blood vessels. Retrieved April 13, 2012, from http://lblackboard.yc.edu/webapps/portal/frameset.jsp?tab_tab_group_id=_2_1&url=%2Fwebapps%2Fblackboard%2Fexecute%2Flauncher%3Dcourse%26id%3D_43466_1
Science News (April
3, 2012).Arteries under pressure early on: mice fed a high-fat diet show signs
of artery damage after only 6 weeks. Retrieved April 12, 2012 from http://www.sciencedaily.com/releases/2012/04/120411102434.htm
Chapter 9 The
Immune System and Mechanisms of Defense
Table of Contents
9.1 Pathogens cause disease
a. Bacteria: Single-celled living
organisms
b. Viruses: Tiny infectious agents
c. Prions: Infectious proteins
d. Transmissibility, mode of
transmission, and virulence determine health risk
9.2 The lymphatic system defends the body
a. Lymphatic vessels transport lymph
b. Lymph nodes cleanse the lymph
c. The spleen cleans the blood
d. Thymus gland hormones cause T
lymphocytes to mature
e. Tonsils protect the throat
9.3 Keeping pathogens out: The first line of defense
a. Skin: An effective deterrent
b. Impeding pathogen entry in areas
not covered by skin
1. Tears, saliva, and
earwax
2. Mucus
3. Digestive and vaginal
acids
4. Vomiting, urination,
and defecation
5. Resident bacteria
9.4 Nonspecific defenses: The second line of defense
a. Phagocytes’ engulf foreign cells
b. Inflammation: Redness, warmth,
swelling, and pain
c. Natural killer cells target
tumors and virus-infected cells
d. The complement system assists
other defense mechanisms
e. Interferon’s interfere with viral
reproduction
f. Fever raises body temperature
9.5 Specific defense mechanisms: The third line of
defense
a. The immune system targets
antigens
b. Lymphocytes are central to
specific defenses
c. B cells: Antibody-mediated
immunity
d. The five classes of antibodies
e. Antibodies’ structure enables
them to bind to specific antigens
f. T cells: Cell-mediated immunity
1. Helper T cells
stimulate other immune cells
2. Memory T cells
reactivate during later exposures
9.6 Immune memory creates immunity
9.7 Medical assistance in the war against pathogens
a. Active immunization: An effective
weapon against pathogens
b. Passive immunization can help
against existing or anticipated infections
c. Monoclonal antibodies:
Laboratory-created for commercial use
d. Antibiotics combat bacteria
9.9 Inappropriate immune system activity causes
problems
a. Allergies: A hypersensitive
immune system
b. Autoimmune disorders: Defective
recognition of “self”
1. Lupus erythematosus: Inflamed connective
tissue
2. Rheumatoid arthritis:
Inflamed synovial membranes
9.1 Pathogens
cause disease
All around us
are bacteria, viruses and prions. Most are harmless and beneficial, but the
ones that cause disease are pathogens.
They come from outside the body to cause us harm. Our immune system and other
general defense mechanisms work to protect us against pathogens (Johnson 2012):
The skin, stomach acid, tears and actions such as vomiting and defecation are
ways of expelling or neutralizing pathogens before they can harm us.
A picture of
Nonspecific defense mechanisms
http://www.slic2.wsu.edu:82/hurlbert/micro101/pages/Chap12.html,
Retrieved April 8, 2012.
Nonspecific defense mechanisms help the body
respond to generalized tissue damage and the common bacteria and some viruses,
Specific defense mechanisms enable the body to recognize and kill specific
bacteria and other foreign cells and to neutralize viruses.
All three mechanisms
work together to protect us from pathogens. The immune system is made up of
cells, proteins, and structures of the lymphatic and circulatory system; it is
only capable of killing or neutralizing pathogens or abnormal cells it
recognizes.
Pathogens include
bacteria, viruses, fungi and a few protozoa and possibly prions (Johnson 2012).
9.1a Bacteria:
Single-celled living organisms
Bacteria are single-celled organisms that do not
have a nucleus or membrane-bound organelles (Johnson 2012). Bacteria can take
on the shape of a sphere, rod or spiral because their outer surface is covered
by a rigid cell wall. Bacteria is smaller than a human cell giving it an
advantage. They contain a higher surface-to-volume ratio making it easier to
obtain raw materials and getting rid of wastes by diffusion. Necessary to
maintain life, grow and divide. Bacteria uses ATP and amino acids for making
proteins the same as a human cell. Bacteria can obtain raw materials anywhere.
Some bacteria break down raw sewage and cause the decomposition of dead animals
and plants (Johnson 2012). Others can obtain nutrients from the soil and air
(Johnson 2012). Through the use of bacteria antibiotics, hormones, vaccines and
genetic engineered foods have been produced. Some bacteria are pathogens that
rely on living human cells for their energy supply and in the process they
damage or kill the human cells. They can cause pneumonia, tonsillitis,
tuberculosis, botulism, toxic shock syndrome, syphilis, Lyme disease and many
other diseases (Johnson 2012). Bacterial infections can be treated with
antibiotics that inhibit or abolish the growth of bacteria, fungi and protozoa.
9.1b Viruses:
Tiny infectious agents
Viruses are smaller much smaller than bacteria
and consist of either RNA or DNA surrounded by a protein coat (Johnson 2012). Viruses
use their DNA or RNA to force a living cell to make more copies of the virus. They
have no organelles so they cannot grow or reproduce. Viruses are dead or alive
it is an ongoing debate; however, they cannot reproduce until they take over a
living cell. The virus uses the cell’s organelles to reproduce.
Viruses can enter
a living cell by entering the cell’s cytoplasm by endocytosis (transporting the virus into a cell by using a coated
vesicle). Once inside the cell the protein coats are dissolved and the viral
genetic material is released for incorporation into the cells’ genetic material
(Johnson 2012). Other viruses merge their outer coat with the cell membrane and
release their genetic contents into the cell’s cytoplasm and other viruses
attach to the outer surface of the cell membrane and inject the genetic
material into the cell (Johnson 2012). The presence of the viral genetic
material causes the cell to begin producing thousands of copies of the virus.
Viral infections can vary in degrees of seriousness depending on a persons’
health and age. Antibiotics generally do not work against viral infections.
9.1c Prions:
Infectious proteins
A picture of a normal prion on the left and a
disease-causing prion on the right.
http://www.scq.ubc.ca/prions-infectious-proteins-repsonsible-for-mad-cow-disease/, Retrieved April 8, 2012.
Prions are normal brain proteins that are not
folded correctly (Oellers, Online Presentation, 2012). Prions destroy nerve
cells in the brain and spinal cord by triggering nearby normal forms of the
protein to misfold as well, causing your body to experience bizarre behaviors.
Eventually so many prions accumulate within infected brain cells that the cells
die and burst, releasing prions to infect other brain cells and causing the
death of nerve cells.
There is no
known cure for prion infection. They resist freezing, drying, and cooking
(Oellers, Online Presentation 2012). Infection occurs when humans eat cattle
that have been infected with mad cows’ disease causing a human disease called
variant Creutzfeldt-Jakob disease (vCJD) (Johnson 2012).
9.1 d
Transmissibility, mode of transmission, and virulence determine health risk
Factors that determine the danger of a pathogen
include
(Johnson 2012):
·
How
easily it is passed from one person to another (mucus to hand, cold)
·
How
it is transmitted (exchange of bodily fluid, food, blood, air)
·
How
damaging the resulting disease is (cold minor, Aids deadly)
9.2 The
lymphatic system defends the body
The lymphatic system performs three
important functions (Johnson 2012):
·
Helps
maintain the volume of blood in the cardiovascular system (by returning excess
fluid back to the capillaries and back to the cardiovascular system)
·
Transports
fats and fat-soluble vitamins absorbed from the digestive system to t he
cardiovascular system
·
Defends
the body against infection
Most of the
cells of the immune system live in the lymphatic system. The basic components
consist of the network of lymph vessels throughout the body, the lymph nodes,
the spleen, the thymus gland, and the tonsils and adenoids (Johnson 2012).
9.23a Lymphatic
vessels transport lymph
The lymphatic
system begins as a network of small, blind ended lymphatic capillaries in the vicinity
of the cells and blood capillaries (Johnson 2012). They contain wide spaces
between overlapping cells allowing them to absorb substances that are too large
to enter a blood capillary like bacteria.
The fluid in the
lymphatic capillaries is called lymph
a milky body fluid that contains WBCs, proteins, fats and can contain bacteria
and viruses. The lymphatic capillaries
merge to form the lymphatic vessels
that consist of three thin layers. The lymphatic vessels merge to form larger
vessels creating two major lymphatic ducts : the right lymphatic duct and
thoracic duct (Johnson 2012).The two lymph ducts join the subclavian veins in
the shoulders and returning the lymph to the cardiovascular system.
9.2b Lymph nodes
cleanse the lymph
Lymph nodes remove microorganisms, cellular debris
and abnormal cells from the lymph before returning it to the cardiovascular
system (Johnson 2012). Lymph nodes are located at intervals along the lymphatic
vessels. There are hundreds of them and can be found in the digestive tract,
neck, armpits and groin (Johnson 2012).
http://www.onplanetearth.com/lymphsystem.jpg,
Retrieved April 8, 2012.
Inside the lymph
nodes is connective tissue and two types of WBC, macrophages and lymphocytes
that identify microorganisms and remove them.
The lymphatic vessels carry lymph into and
out of each node in one direction by the used of one-way valves. As the fluid
flows through a node, the macrophages destroy foreign cells by phagocytosis and
the lymphocytes activate other defense mechanisms (Johnson 2012). The clean lymph
fluid flows out of the node and continues to the veins.
9.2c The spleen
cleanses blood
The spleen is the largest lymphatic organ.
It is soft, fist sized mass located in the upper-left abdominal cavity (Johnson
2012).
The organ is filled with two types of tissue (Johnson 2012):
1.
Red pulp contains
macrophages that scavenge and break down microorganisms and damaged RBCs and
platelets. Clean blood is stored here.
2.
White pulp contains
lymphocytes that search for foreign pathogens.
The spleen has two main functions (Johnson 2012):
1.
Controls
the quality of circulating red blood cells, by removing the old and damaged
ones.
2.
Helps
fight infection.
Infections such
as leukemia can enlarge the spleen
and can cause it to rupture causing internal bleeding. Surgery is necessary to
remove the spleen. We can live without a spleen because our lymph glands, liver
and red bone marrow aid in circulating RBCs, removing them and fighting
infection.
9.2d Thymus
gland hormones cause T lymphocytes to mature
The thymus gland
plays a key role in the body’s immune response. Science Daily (March 29, 2012) state
in their article, that researchers have generated artificially thymus tissue in
a mouse embryo to enable the maturation of immune cells.
The thymus gland facilitates maturation of
T lymphocytes (Oellers, Online Presentation, 2012).
The thymus gland secretes two hormones (Johnson 2012):
1.
Thymosin
2.
Thymopoietin
These two
hormones cause lymphocytes called T
(cells) to mature and take on specific defenses. The thymus gland varies in
size according to age. It is largest and most active during childhood. As we
age our thymus gland stops growing and begins to shrink and can eventually
disappear to be replaced by fibrous and fatty tissue. The thymus gland is found
in the lower neck, behind the sternum and just above the heart (Johnson 2012).
9.2e Tonsils
protect the throat
Lymphocytes in
the tonsils gather and filter out many microorganisms that enter the throat in
food and air (Johnson 2012). Tonsils
are lymphatic tissue located near the entrance of the throat and along with
adenoids they protect the throat (Oellers, Online Presentation, 2012).
Adenoids are lymphatic tissue that if continued
to enlarge obstruct airflow from nose to throat causing mouth breathing, a
nasal voice and snoring. Adenoids usually disappear by puberty, but can
continue to grow and cause problems.
9.3 Keeping
pathogens out: The first line of defense
Our bodies have
several ways to prevent pathogens from entering into our bodies: Our skin,
tears, saliva, earwax, mucus, to name some of the few.
9.3a Skin: An
effective deterrent
The skin is the most important barrier to
keep pathogens out.
The skin has four key attributes that make it an
effective barrier
(Johnson 2012):
1.
Structure.
The outer most layer of our skin is called keratin
(fingernails are made of). Keratin forms a tough elastic barrier keeping
microorganisms at bay.
2.
Constantly
being replaced meaning that any pathogens deposited on the surface of the skin
are shed along with the dead cells.
3.
Acidic
pH because of sweat glands producing sweat.
4.
Production
of an antibiotic by sweat glands called dermicidin
kills harmful bacteria.
9.3b Impeding
pathogen entry in areas not covered by skin
Pathogens are
most effective when entering our bodies through moist surfaces such as mucous membranes that line the
digestive, urinary, respiratory and reproductive tracts along with the eyes and
ears.
These moist
areas have defenses to block pathogens from entering into our bodies such as
tears, saliva, earwax, mucus, vomiting, urination and defecation to name the
few.
9.3b, 1 Tears,
saliva and earwax
Tears lubricate the eyes while washing away
particles. Tears and saliva contain lysozyme,
which is an enzyme that kills many bacteria (Johnson 2012). Saliva lubricates the tissues inside of
the mouth and rinses microorganisms from the mouth into the stomach where
stomach acid destroys them. Earwax
traps small particles and microorganisms.
9.3b, 2 Mucus
Mucus is sticky and secreted by cells like
the lining of the digestive tract and the airways of the respiratory system.
Mucous binds microorganisms to itself so that it cannot enter our bodies. Our bodies
get rid of the mucous by cilia (hair
like projections) in our airways that sweep the mucus toward our throat where
we cough or swallow the mucus containing the microorganism (Johnson 2012).
9.3b, 3
Digestive and vaginal acids
Vaginal secretions are slightly acidic, but not
anything like a digestive tract that is undiluted. It strong enough to kill
nearly all pathogens that enter on an empty stomach. Bacteria called
Helicobacter pylori that have evolved to endure the stomach acid cause a stomach ulcer.
9.3b, 4
Vomiting, urination, and defecation
Vomiting is a way for the body to get rid of
toxin or microorganisms.
The urinary system is slightly acidic and
constantly flushing of urination keeps bacteria low.
Defecation helps remove microorganisms from the
digestive tract. Diarrhea is caused
by an illness where the muscles in the intestinal wall start to contract rapidly
and the intestines secrete additional fluid into the feces (Johnson 2012).
9.3b, 5 Resident
bacteria
Beneficial bacterial often reside in
the mucous membranes lining the vagina and the digestive tract. They help
control population levels of harmful organisms by competing for food and
winning. They also lower the vagina pH levels where many fungi and bacteria
cannot survive.
9.4 Nonspecific
defenses: The second line of defense
Nonspecific defense mechanisms include the immune
system cells that engulf and digest foreign cells, chemicals that are toxic to
foreign cells, proteins that interfere with viral reproduction, and the
development of a fever (Johnson 2012).
Our second line
of defense do not target specific pathogens but respond to all.
Nonspecific
defenses include phagocytes, natural killer cells, the inflammatory response,
the complement system, interferon’s’ and fever.
9.4a Phagocytes
engulf foreign cells
Phagocytes are white blood cells that surround and
engulf invading bacteria (Oellers, Online Presentation 2012). This is a process
known as phagocytosis (Johnson 2012). Phagocytosis
begins when the phagocyte captures the bacterium, surrounds it and encloses the
bacterium in a membrane-bound vesicle. Inside the cell, the vesicle fuses with lysosomes,
which dissolve the bacterial membranes, and the wastes and debris are
discarded.
Neurtophils and
macrophages and eosinophils are types of phagocytes.
Neutrophils are the first white blood cells to
respond to infection (Johnson 2012). They digest and destroy bacteria and some
foreign fungi in the blood and tissue fluids.
Monocytes are white blood cells that leave the
vascular system enter the tissue fluids and develop into macrophages. Macrophages engulf and digest large
numbers of foreign cells including viruses and bacterial parasites. Macrophages
also scavenge old blood cells, dead tissue fragments and cellular debris as a
tool for cleanup (Johnson 2012). Macrophages create new white blood cells by
releasing a chemical that stimulates production of white blood cells.
Eosinophils engulf and digest invaders that are too
big for the other phagocytes. They accomplish this by bombarding large parasites
with digestive enzymes.
White blood
cells increase when the body is fighting infection. Tissue fluid, dead
phagocytes and microorganisms and cellular debris accumulate at the infection
sited producing pus. An abscess forms
when pus becomes trapped and the body forms skin over the infected areas.
Common places for abscesses are the breast (mastitis, the gums (dental
abscesses) and the liver or brain. You can drain an abscess or some require
that you take antibiotic drugs or surgical removal to get rid of an abscess.
9.4b Inflammation:
Redness, warmth, swelling and pain
Inflammation has four outward signs (Johnson 2012):
1.
Redness
2.
Warmth
3.
Swelling
4.
Pain
These events
prevent damage from spreading, dispose of cellular debris and pathogens and aid
in tissue repair mechanisms.
When tissue is
damaged the inflammatory process begins. Chemicals bare released from the
damaged cells; this begins the process. These chemicals stimulate mast cells
which are connective tissue cells specialized to release histamine. Histamine promotes dilation of
neighboring blood vessels.
White blood
cells are too big to cross capillary walls. Histamine makes it possible for
WBCs to squeeze through the walls into the interstitial fluid where they attack
foreign organisms and damaged cells. The dilation of blood vessels brings more
blood into the injured area making it red
and warm. The rising temperature
increases phagocyte activity. Swelling
is caused by the capillary walls allowing more fluid to seep into the tissue
spaces. This extra fluid dilutes pathogens and toxins and brings in clotting
proteins that form a fibrin mesh to wall off the damaged areas from healthy
tissue (Johnson 2012). The extra fluid also carries in extra oxygen and
nutrients to promote in the healing of tissue and carries away dead cells,
microorganisms and other debris from the area.
Pain forces the injured person to rest to
aid in the healing process. Pain is caused by the swollen tissue pressing
against nerve endings.
9.4c Natural
killer cells target tumors and virus-infected cells
Natural killer (NK) cells are a type of
lymphocytes (white blood cells) that attacks tumor cells and viruses (infected
cells) (Oellers, Online Presentation, 2012). NK cells are not phagocytes; instead,
they release chemicals that break down their targets’ cell membranes. They are
able to recognize certain changes that take place in the plasma membranes of
tumor cells and virus-infected cells. The target of a NK cells destroys the cell’s
nucleus and the target cell’s membranes develop holes. The NK cells aid in the
inflammatory response by secreting substances.
9.4d The
complement system assists other defense mechanisms
The complement system is made up of
approximately 20 plasma proteins that assist other defense mechanisms by
circulating in the blood (Johnson 2012). Once activated the protein than
activates another protein and so on creating a domino effect. Some activated
proteins can join to form large protein complexes that create holes in
bacterial cell walls causing them to swell and burst. Other activated
complement proteins bind to bacterial cell membranes, marking them for
destruction by phagocytes. Others stimulate mast cells to release histamine or
serve as chemical attractants to draw additional phagocytes to the infection.
9.4e Interferons
interfere with viral reproduction
Viruses cannot
reproduce on their own; they must invade a host’s cell in order to reproduce.
Cells that
become infected by viruses secrete a group of proteins call interferons (Johnson 2012). Interferons
diffuse to nearby healthy cells and bind to their cell membranes. They then
stimulate the healthy cells to produce proteins that interfere with the
reproduction of viral proteins making it harder for viruses to infect the
protected cell.
Interferon
proteins can protect against viral diseases such as genital warts, hepatitis B
and one form of leukemia (Johnson 2012).
9.4f Fever
raises body temperature
A normal body
temperature is 98.6 F. When macrophages detect and attract bacteria, viruses,
or other foreign substances, they release certain chemicals into the
bloodstream called pyrogens (Johnson 2012). Pyrogens cause the brain to raise your body temperature. Modest
fevers help the body to fight infection by increasing the metabolic rate of
body cells, speeding up both defense
mechanisms and tissue-repair processes. When the infection is gone
macrophages stop releasing pyrogens and your body temperature returns to
normal. Abnormally high fevers can be dangerous in adults. If your core
temperature reaches 105 F your brain begins to fry; seek medical attention.
9.5 Specific
defense mechanisms: The third line of defense
Specific defense mechanisms involve the
production of antibodies and T cells that recognize and inactivate one specific
pathogen. Specific defense mechanisms have a memory component that remembers
initial exposure and responds more quickly and aggressively on subsequent
exposures (Oellers, Online Presentation 2012).
The immune system is made up of cells,
proteins and the lymphatic system that work together to detect and kill
particular pathogens and abnormal body cells.
9.5a The immune
system target antigens
http://www.lymphedemapeople.com/thesite/lymphedema_lymphatic_system_and_immunity.htm,
Retrieved April 8, 2012.
An antigen is any substance that triggers
an immune response (Oellers, Online Presentation, 2012). The immune system
responds to each uniquely shaped antigen by producing specific antibodies to
attack and inactivate the antigen.
All antigens are
located on the outer surface of a cell or virus. Human cells have unique
proteins on the surfaces that our immune system uses to recognize that the
cells belong to us. These are self-markers known as major histocompatibility complex (MHC) proteins. Each person has a unique
set of MHC proteins that would act as antigens in another person’s body.
9.5b Lymphocytes
are central to specific defenses
Lymphocytes are white blood cells that synthesize
from stem cells in bone marrow. Found in the bloodstream, tonsils, spleen,
lymph nodes and thymus gland they total about 30% of circulating WBCs (Johnson
2012).
There are two types of lymphocytes (Johnson 2012):
http://classes.midlandstech.com/carterp/Courses/bio225/chap17/lecture4.htm,
Retrieved April 8, 2012.
1.
B
cells
2.
T
cells
B cells mature in bone marrow and are
responsible for antibody-mediated immunity. In other words, they produce
antibodies (proteins that bind with and neutralize specific antigens). B cells
protect us best from viruses, bacteria and foreign molecules that are soluble
in blood and lymph, because B cells release antibodies into the lymph,
bloodstream and tissue fluid.
T cells mature in the thymus gland and are responsible
for cell-mediated immunity. T cells directly attack foreign cells, coordinate
the immune response from other cells, are active against parasites, fungi,
viruses, intercellular bacteria, cancer cells, and cells with “non-self” MHC
(Oellers, Online Presentation, 2012).
9.5c B cells:
Antibody-mediated immunity
As B cells mature,
they develop unique surface receptors that allow them to recognize specific
antigens. When a B cell encounters a surface antigen with the matching receptor,
it activates the B cell’s surface receptors and bind to the antigen. The B cell
begins to grow and multiply producing more B cells exactly like the original
with the same surface receptors called clones.
Some of the clone cells become memory cells that
lie in wait for the next exposure to the antigen and other clone cells become
plasma cells. Plasma cells secrete
antibodies into the lymph fluid and ultimately into the blood plasma.
9.5d The five
classes of antibodies
Antibodies belong to the class of blood plasma proteins
called gamma globulins also known as
immunoglobulin (Ig) (Johnson 2012).
There are five classes of Ig:
http://www.beltina.org/health-dictionary/immunoglobulin-a-d-e-g-m-ida-igd-ige-igg-igm-therapy.html, Retrieved April 8, 2012.
1.
IgG are the most
prevalent in blood. They are found in blood, lymph, intestines and tissue
fluid. They activate the complement system and neutralize any toxins. They are
the only antibodies that cross the placenta during pregnancy and pass on the
mother’s acquired immunities to the fetus.
2.
IgM are the
antibodies that are the first to be released during immune responses. Found in
blood and lymph, they activate the complement system and cause foreign cells to
clot.
3.
IgA are antibodies that
enter areas of the body covered by mucous membranes, such as the digestive,
reproductive, and respiratory tracts. There they neutralize pathogens. They are
also present in mother’s milk and are transmitted to the infant during
breast-feeding.
4.
IgD are antibodies
in the blood, lymph, and B cells. Their function is not clear.
5.
IgE are the rarest of the antibodies. They are in
B cells, mast cells and basophils. They activate the inflammatory response by
triggering the release of histamine. They also trigger allergic responses.
9.5e Antibodies’
structure enables them to bind to specific antigens
All antibodies
share the same basic structure that consist of four linked polypeptide chains
arranged in a Y shape. Each of the four chains has a constant region that forms
the trunk and two branches and a variable region that represents the
antigen-binding site (Johnson 2012). Each variable region has a unique shape
that fits only one specific antigen.
9.5f T cells:
Cell-mediated immunity
There are two basic functional differences between B
cells and T cells
(Johnson 2012):
1.
B
cells produce circulating antibodies
2.
T
cells either release chemicals that stimulate other cells of the immune system
or they directly attack the foreign cell and kill it.
T cells originate from stem cells in bone
marrow and mature in the thymus (Oellers, Online Presentation, 2012).
Macrophages and
activated B cells act as antigen-presenting
cells (APCs) that engulf foreign particles, then lysosomes partially digest
the pathogen. A vesicle containing MHC molecules binds to the digestive vesicle
and a fragment of the antigen form an antigen MHC complex that is displayed on
the surface of the cell when the vesicle fuses with the cell membrane and
releases its digestive products. T cells recognize fragments of the antigen
along with its own cell-surface self marker.
T cells develop two sets of surface proteins once
they mature (Oellers,
Online Presentatino, 2012):
1.
CD4 T cells are memory and helper cells
2.
CD8 T cells will become
cytotoxic and suppressor cells
These proteins
determine what type of T cell they will become.
9.5f, 1 Helper T cells stimulate other immune cells
CD4 becomes a helper T cell when its
receptors encounter an antigen-presenting cell displaying a fragment of an
antigen. This new T cell undergoes mitosis producing a clone which recognizes
the same antigen. Most of the cells in the helper T cell clone will secrete cytokines, which stimulate other immune
cells such as phagocytes, natural killer cells, and T cells with CD8 receptors.
Helper T cells are crucial to an effective
immune response. Without them the immune response would be nonexistent. AIDS is
so devastating because HIV destroys helper T cells, weakening the body’s
ability to mount a cell-mediated immune response (Johnson 2012).
Cytotoxic T cells are the only T cells that
directly attack and destroy other cells. Cytotoxic T cells are produced when a
mature T cell with CD8 receptors meets an antigen-producing cell that displays
an antigen fragment.
When a cytotoxic
T cell is activated it locates and binds to a target cell, secretary vesicles
release a protein called perforin into the space between the two cells (Johnson
2012). The perforin molecules
assemble themselves into a pore in the target cell, allowing water and salts to
enter. This will eventually kill the cell. The cytotoix T cell also releases granzyme, a toxic enzyme that is small
enough to pass through the pore (Johnson 2012). Then it detaches from the
target cell and goes off in search of other prey.
9.5f, 2 Memory T
cells reactivate during later exposures
Memory cells are reactivated when an antigen that
originally stimulated their production is presented to them again. Memory T
cells are an important factor that distinguishes specific defenses from
nonspecific defense mechanisms.
9.6 Immune memory creates immunity
Your first
exposure to a particular antigen generates a primary immune response. This involves recognition of the antigen
and production of B and T cells. The primary immune response takes three to six
days after the antigen first appears to start synthesizing specific B cells.
Antibodies reach their peak about 10-12 days after first exposure (Johnson
2012).
B and T cells
create memory cells this is the basis for immunity from disease. Secondary immune response kicks in when
the initial antigen pops up again. This time however within hours after the
exposure to the same antigen memory cells bind to the pathogen. Within a few
days antibodies respond.
Why can a person
get a cold or flu over and over again? The reason being is that the cold and
flu are viruses that evolve rapidly changing every year. Their antigens change
enough that each one requires a different antibody and each exposure triggers a
primary response.
9.7 Medical
assistance in the war against pathogens
Through medicine,
we have been able to produce medicines and vaccines to help us combat
pathogens. Immunizations help the
body resist specific pathogens.
9.7a Active
immunization: An effective weapon against pathogens
Vaccines are a strategy for causing the body to
develop immunity to a specific pathogen (Oellers, Online Presentation, 2012). This
way when we are introduced to the pathogen again our secondary immune response
will activate shielding us from the danger of the disease.
The process of
activating the body’s immune system in advance is called active immunization (Johnson 2012). There are issues of safety,
time and expense when it comes to vaccines.
First, vaccines are produced from dead or weakened pathogens for example
the polio vaccine made from weakened poliovirus. Vaccines that are made from
live, but weakened pathogens make better vaccines because they eject a greater
immune response; however, this type of vaccine can cause the disease itself.
Second, a vaccine confers immunity against only one pathogen, so a different
vaccine is needed for every virus. Third, vaccines do not cure an existing
disease.
Active
immunizations produce long-lived immunity that can protect us for many years.
The widespread practice of vaccinations has greatly reduced many diseases such
as polio, measles and whooping cough (Johnson 2012).
9.7b Passive
immunization can help against existing or anticipated infections
Passive immunization is
administering protective antibodies to an individual (Oellers, Online
Presentation, 2012). This type of immunization produces short-term protection
because the administered antibodies disappear from the circulation quickly
because the person’s own B cells aren’t activated and so memory cells for the
pathogen do not develop.
Passive
immunizations has been used effectively against common viral infections like
hepatitis B and measles.
9.7c Monoclonal
antibodies: Laboratory-created for commercial use
Monoclonal antibodies are produced in
the laboratory from cloned descendants of a single hybrid B cell (Johnson
2012). They are antibodies that are made specific for a single antigen.
Monoclonal
antibodies are synthesized by immunizing a mouse with a specific antigen. Then
extracting the B cells from the mouse’s spleen and fusing antibody-producing B
cells with cancer (myeloma) cells to
produce fast-growing cells. The desired antibody is the separated out and
cloned producing millions of copies. This is why monoclonal antibodies are
proving useful in research, testing and cancer treatments because they are pure
and they can be produce cheaply in large quantities.
Monoclonal
antibodies are used in home pregnancy tests, screening for prostate cancer and
diagnostic testing for hepatitis, influenza and HIV/AIDS (Johnson 2012).
9.7d Antibiotics
combat bacteria
Antibiotic means against life (Johnson 2012). Antibiotics kill bacteria or stop their
growth. The difference between bacteria and human cells is that bacteria have a
thick cell wall and human cells do not. Bacterial DNA is not safely enclosed in
a nucleus, human DNA is, and bacterial ribosome’s are smaller than human ribosome’s.
Bacterial rate of protein synthesis is very rapid and they grow and divide.
Antibiotics are ineffective against viruses they can only combat against
bacteria. Most antibiotics kill bacteria by interfering with bacterial protein
synthesis or bacterial cell wall synthesis.
9.9
Inappropriate immune system activity causes problems
Inappropriate immune system activity can
lead to allergies and autoimmune diseases such as lupus erythematosus and
rheumatoid arthritis.
9.9a Allergies:
A hypersensitive immune system
10% of North
Americans suffer from allergies (Johnson 2012). Allergies are hypersensitivity
reactions (Oellers, Online Presentation 2012).
An allergy is an inappropriate response of
the immune system to an allergen. An
allergen is any substance (antigen) that causes an allergic reaction (not a
pathogen, but the body reacts, as though it is a pathogen) (Oellers, Online
Presentation, 2012). Exposure to an allergen triggers a primary immune
response, causing B cells to produce specific IgE (allergic reactions fall into
this group) antibodies. The IgE antibodies bind to mast cells (found in
connective tissue) and to circulating basophiles.
When the same allergen
enters the body a second time, it binds to the IgE, antibodies on mast cells
and basophiles, causing them to release histamine. The result is an allergic reaction, a typical inflammatory
response that includes warmth, redness, swelling, and pain in the area of
contact with the allergen (Johnson 2012).
Some allergens
affect only the areas exposed others include food allergens and bee sting venom
are absorbed or injected into the bloodstream. Such allergens elicit a systemic response meaning they affect
several organ systems. Systemic responses include constriction of smooth muscle
in the lungs making it difficult to breathe and digestive system and dilation
of blood vessels (Johnson 2012).
When the circulatory
collapses with a life threatening fall in blood pressure this is known as anaphylactic shock (Johnson 2012).
People with this condition should be rushed to the hospital because the
reaction can be fatal. People who know that they have allergic reactions such
as to bee stings are advised to carry an emergency kit with them that contains
a self-injected hypodermic needle of epinephrine, a hormone that dilates the
airway and constricts peripheral blood vessels, preventing shock.
9.9b Autoimmune
disorders: Defective recognition of “self”
The immune
system’s on occasion can fail to distinguish self from nonself. When this
happens the immune system produces antibodies and cytotoxic T cell that target
its own cells (Johnson 2012). Autoimmune
disorders are conditions that result from this happening. At the moment
there are no cures for autoimmune disorders. Treatments include therapies that
depress the body’s defense mechanisms and relieve the symptoms. Autoimmune
conditions include multiple sclerosis, a progressive disorder of
the central nervous system, Type 1
diabetes mellitus, which targets cell in the pancreas, lupus erythematosus and rheumatoid
arthritis.
9.9b, 1 Lupus
erythematosus: Inflamed connective tissue
Lupus is an autoimmune disorder in which the
body attacks its own connective tissue (Johnson 2012). One type of lupus called
discoid lupus erythematosus
primarily affects areas of the skin exposed to sunlight. Systemic lupus erythematosus affects the heart, blood vessels, lungs,
kidneys, joints and brain. Lupus often starts as a red skin rash on the face or
head and can include fever, fatigue, joint pain and weight loss. Spreading
inflammation can lead to osteoarthritis, pericarditis or pleurisy (inflammation
of the lining of the lungs). Medications can reduce the inflammation and
alleviate the symptoms.
9.9b, 2
Rheumatoid arthritis: Inflamed synovial membranes
Rheumatoid arthritis is a type of
arthritis involving inflammation of the synovial membrane that lines certain
joints (Johnson 2012). At first, fingers, wrists, toes or other joints become
painful and still. Over time the inflammation destroys joint cartilage and the
neighboring bone. Eventually bony tissue begins to break down and fuse
resulting in deformities and reduced range of motion. The disease is
intermittent, but with each recurrence the damage is progressively worse.
Pain-relieving medications can help, as can regular mild exercise and physical
therapy to improve range of motion.
REFERENCES
Johnson, M. D. (2012, 2010, 2008).
Human Biology: concepts and current issues, sixth edition. Pearson Education,
inc.; Benjamin Cummings.
Oellers, J. (n.d). Online
Presentation: Ch. 9 The immune system and mechanisms of defense. Retrieved
April 8, 2012, from http://lblackboard.yc.edu/webapps/portal/frameset.jsp?tab_tab_group_id=_2_1&url=%2Fwebapps%2Fblackboard%2Fexecute%2Flauncher%3Dcourse%26id%3D_43466_1
Science News (March 29, 2012).Artificial
thymus tissue enables maturation of immune cells. Retrieved April 12, 2012 from
http://www.sciencedaily.com/releases/2012/04/120411102434.htm
Ch. 10 The
Respiratory System: Exchange of Gases
Table of Contents
10.1 Respiration takes place throughout the body
10.2 The respiratory system consists of upper and
lower respiratory tracts
a. The upper respiratory tract
filters, warms, and humidifies air
b. The lower respiratory tract
exchanges gases
1. The larynx produces
sound
2. Bronchi branch into
the lungs
3. The lungs are organs
of gas exchange
4. Gas exchange occurs
in alveoli
5. Pulmonary capillaries
bring blood and air into close contact
10.3 The Process of breathing involves a pressure
gradient
a. Inspiration brings in air,
expiration expels it
b. Lung volumes and vital capacity
measure lung function
10.4 Gas exchange and transport occur passively
a. Gases diffuse according to their
partial pressures
b. External respiration: The
exchange of gases between air and blood
c. Internal respiration: The
exchange of gases with tissue fluids
d. Hemoglobin transports most oxygen
molecules
e. Most Carbon Dioxide is
transported in plasma as bicarbonate
10.5 The nervous system regulates breathing
a. A respiratory center establishes
rhythm of breathing
b. Chemical receptors monitor carbon
dioxide, hydrogen and oxygen levels
c. We can exert some conscious
control
10.6 Disorders of the respiratory system
a. Reduced airflow or gas exchange
impedes respiratory function
1. Asthma: Spasmodic
contraction of bronchi
2. Emphysema: Alveoli
become permanently impaired
3. Bronchitis:
Inflammation of the bronchi
4. Cystic fibrosis: An
inherited condition
b. Microorganisms can cause
respiratory disorders
1. Colds and the flu:
Common viral respiratory tract infections
2. Pneumonia: Infection
inflames the lungs
3. Tuberculosis:
Bacterial infection scars the lungs
4. Botulism: Poisoning
by bacterial toxin
c. Lung cancer is caused by
proliferation of abnormal cells
d. Pneumothorax and atalectasis: A
failure of gas exchange
e. Congestive heart failure impairs
lung function
10.1 Respiration
takes place throughout the body
The function of
the respiratory system is to
exchange these gases (oxygen and carbon dioxide) with the air (Johnson 2012).
We extract oxygen from the air we breathe and exhale carbon dioxide, the waste
product of our metabolism. The oxygen in the air comes from the plants. The
plants absorb carbon dioxide through their leaves and use it to accomplish
photosynthesis (turning carbon dioxide into oxygen).
Respiration includes four processes (Oellers,
Online Presentation, 2012):
1.
Breathing
(ventilation) is the movement of air
into and out of the lungs and uses associated bones, muscles and nerves to
accomplish this.
2.
External
respiration
is the exchange of gases between inhaled air and blood that takes place in the
lungs.
3.
Internal
respiration is
the exchange of gases between the blood and tissue fluids.
4.
Cellular
respiration
is the process of using oxygen to produce ATP within cells. Cellular
respiration generates carbon dioxide as a waste product.
The respiratory
system is also responsible for the production of sound (vocalization).
10.2 The
respiratory system consists of upper and lower respiratory tracts
http://www.emc.maricopa.edu/faculty/farabee/biobk/biobookrespsys.html,
Retrieved April 14, 2012.
The respiratory
system is divided into the upper and lower respiratory tracts.
The upper respiratory tract includes (Oellers,
Online Presentation, 2012):
·
The
nose (passageway for air) and nasal cavity (filters, warms and
moistens air)
·
Pharynx (throat) is the
common passageway for air, food and liquid. The pharynx is located above the
“Adam’s apple” in your neck.
The lower respiratory tract includes (Oellers,
Online Presentation 2012):
·
Larynx (voice box) is
used for the production of sound.
·
Trachea (windpipe) is
the main airway.
·
Bronchi are branching
airways that stem from the trachea.
·
Lungs is the organ of
gas exchange.
10.2a The upper
respiratory tract filters, warms, and humidifies air
The nose is not just used as a passageway for air,
but has many purposes
(Johnson 2012):
·
Contains
receptors for the sense of smell
·
Filters
inhaled air and screens out some foreign particles.
·
Moistens
and warms incoming air.
·
Provides
a resonating chamber that helps give your voice its characteristic tone
The outer
portion of the nose is called the external
nose, while the internal area of the nose is known as the nasal cavity. The outer area of the
nose is made up of cartilage in the front and two nasal bones behind the
cartilage.
The external
nose and nasal cavity are divided into two chambers by the nasal septum (Johnson 2012). Air enters through the nostrils and is
filtered partially by the nose hairs. The air then flows into the nasal cavity,
which is lined with moist epithelial tissue that is supplied with blood
vessels. These blood vessels help to warm incoming air and the epithelial tissue secretes mucus, which
humidifies the air (Johnson 2012). Cilia
are tiny hair like projections that cover the epithelial tissue.
Mucus in the
nasal cavity trap dust, pathogens and other particles in the air, before they
enter further into the respiratory tract. The cilia move the mucus toward the
back of the nasal cavity and pharynx by creating gentle movement back and forth.
There the mucus is coughed out or swallowed where it is digested by stomach
acid. In cold weather, your nose is likely to run because the cilia in the
nasal cavity slow down and allows mucus to pool in the nasal cavity and drip
from the nostrils.
Sinuses are the air spaces inside the skull
lined with tissue that secretes mucus to help trap foreign particles. The
sinuses drain into the nasal cavity by small passageways. Two tear ducts that carry
fluid away from the eyes, drain into the nasal cavity as well. Excessive tears
will also makes your nose “runny” because of the passageways from the sinuses
to the nasal cavity.
Incoming air
enters the pharynx (throat) next. The pharynx
connects the mouth and nasal cavity to the larynx
(voice box) (Johnson 2012). The upper pharynx extends from the nasal cavity to
the roof of the mouth. Into it, open the two auditory tubes (Eustachian tubes) that drain the middle
ear cavities and equalize air pressure between the middle ear and outside air
(Johnson 2012). The lower pharynx is a common passageway for both food and air.
Food passes through the pharynx to the esophagus, and air flows through to the
lower respiratory tract.
10.2b The lower
respiratory tract exchanges gases
The lower respiratory tract includes (Johnson 2012):
·
Larynx
·
Trachea
·
Bronchi
·
Lungs
with bronchioles and alveoli
10.2 b, 1 The
larynx produces sound
The larynx or
voice box extends two inches below the throat.
The voice boxes purpose is to (Johnson 2012):
·
Maintain
an open airway.
·
Route
food and air into the appropriate channels
·
Assist
in the production of sound.
The voice box contains the epiglottis, a flap of cartilage located
at the opening to the voice box. When air flows, through the pharynx the
epiglottis is open, but when we swallow food or liquids the epiglottis blocks
the opening, resulting in food and beverages into the esophagus and digestive
system than into the trachea.
The vocal cords
consist of two folds of connective tissue that extend across the airway (Johnson
2012). The glottis is surrounded by
vocal cords and is the opening to the airway. Ligaments support the vocal cords.
The skeletal
muscles control how tightly the vocal cords are stretched which produces the
unique sounds of our voices. The vibration of the vocal cords makes the sound.
When we are not talking, our vocal cords are relaxed and open, but when we
start to talk they stretch tightly across the tracheal opening, and the flow of
air past the vocal cords cause them to vibrate (Johnson 2012).
The volume of
pitch we have in our voices is contributed to the tension on our vocal cords. High-pitched
tones are from cords that are short and stretched tightly and vice versa with
deep pitched voices. Testosterone in men contributes to them having a deep
voice. In puberty, testosterone causes the larynx to enlarge at puberty
adjusting the tension on their vocal cords.
The mouth,
throat, nose and nasal cavity, tongue and teeth also determine our distinct
voices (Johnson 2012). Muscles in the throat, tongue, soft palate, and lips
create sounds. The throat, nose and nasal sinuses serve as resonating chambers
to amplify tones.
10.2 b, 2 The
trachea transports air
The trachea is the windpipe that extends
from the larynx to the left and right bronchi. The trachea transports air to
and from the lungs (Oellers, Online Presentation 2012). The trachea consists of
smooth muscle and layers of epithelial and connective tissue held open by
tough, flexible C-shaped bands of cartilage (Johnson 2012).
The C-shaped
bands keep the trachea open at all times and permit the trachea to change
diameter when we cough or breathe heavily due to the bands being an incomplete
circle.
The trachea is
lined with cilia covered epithelial tissue that secretes mucus.
Choking occurs
when a foreign object is lodged in the trachea. If the airway is completely
blocked death can occur. Choking stimulates receptors in the throat that trigger
the cough reflex. This is a sudden expulsion of air from the lungs in an
attempt to dislodge foreign object (Johnson 2012).
10.2, b 3
Bronchi branch into the lungs
http://training.seer.cancer.gov/anatomy/respiratory/passages/bronchi.html,
Retrieved April 14, 2012.
The trachea
branches into two airways called the right and left bronchi as it enters the
lung cavity. Bronchioles are small
airways that lack cartilage. The walls of bronchi contain fibrous connective
tissue and smooth muscle reinforced with cartilage. As the airways get smaller
and smaller the cartilage decreases.
The bronchi and bronchioles have many functions: (Johnson 2012)
·
Transport
air.
·
Clean
the air.
·
Warm
the air to body temperature.
·
Saturate
air with water vapor before it reaches the lungs.
Smoking is
terrible on the respiratory tract. It irritates it, destroys the cilia allowing
mucus and debris from the smoke to accumulate in the airway, resulting in
“Smoker’s cough”. Coughing is the body’s way to dislodge a foreign object or
mucus in this case from the airway. Accumulation of mucus leads to frequent
infections because pathogens and irritants remain in the respiratory tract
(Johnson 2012).
10.2b, 4 The
lungs are organs of gas exchange
http://www.picsearch.com/imageDetail.cgi?id=QP55nfR2ekA5C3rpdZqd7L4ieI20s2aa9bg47WXNGSw&width=1663&start=1&q=bronchi,%20bronchioles%20and%20blood%20vessels,%20pleural%20membranes, Retrieved April 14, 2012.
The lungs
consist of supportive tissue that encloses the bronchi, bronchioles, blood vessels
and the areas where gas exchange occurs (Johnson 2012). The heart is what separates
the right lung from the left. Each lung is enclosed in two layers of thin
epithelial membranes called the pleural
membranes. One layer represents the outer lung surface and the other layer
contains a small amount of watery fluid that reduces friction between the
pleural membranes as the lungs and chest wall move during breathing. Pleurisy is the inflammation of the
pleural membranes resulting in a decrease in the secretion of pleural fluid,
increase friction and cause pain during breathing (Johnson 2012). The lungs
consist of several lobes that can be surgically removed without eliminating lung
function. The right lungs consist of three lobes and the left lung two. Each
lobe contains a branching tree of bronchioles and blood vessels.
10.2b, 5 Gas
exchange occurs in alveoli
Lungs are very
soft and mostly consist of air. The lungs
are a system of branching airways that end in 300 million tiny air-filled sacs
called alveoli (Johnson 2012). Alveoli
is where the gas exchange takes place. A
single alveolus is a thin bubble of living squamous epithelial cells only one
cell layer thick. Within each alveolus, certain epithelial cells secrete a
lipoprotein called surfactant that
coats the interior of the alveoli and reduces surface tension that is caused by
the attraction of water molecules toward each other. Without surface tension,
the alveoli could collapse.
10.2b, 6
Pulmonary capillaries bring blood and air into close contact
http://www.picsearch.com/imageDetail.cgi?id=zAaBDgpC5sKwvodUQ42FC8wyC7C4n4x6BzmXDeM-HFQ&width=1663&start=1&q=pulmonary%20capillaries, Retrieved April 14, 2012.
Gas exchange
occurs between the alveoli and pulmonary capillaries. The right ventricle of
the heart pumps deoxygenated blood into the pulmonary trunk, which splits into the left and right pulmonary
arteries. These arteries become smaller and turn into arterioles, eventually
terminating in a capillary bed called the pulmonary
capillaries. Only the squamous epithelial cell of the alveolus and the cell
of the capillary wall separate blood from air (Johnson 2012). Veins then collect the oxygenated blood
from the pulmonary capillaries and return the blood to the left side of the
heart where it is transported to all parts of the body. Heart attacks occur
when the blood vessels going to the heart become filled up with plaque and the
heart is not getting enough oxygen to fulfill its duties. More than 30% of the
one million heart attack victims in the U.S. each year die before seeking
medical attention. Science Daily (April 13, 2012) writes in their article that researchers
are studying the benefits of the AngelMed Guardian and implantable medical
device. This device is currently undergoing clinical trials that alert users
about potential heart attacks through a combination of vibrations, audible
tones and visual warnings.
10.3 The process
of breathing involves a pressure gradient
Breathing
consists of getting air into and out of the lungs; this requires muscular
effort. Since the lungs do not contain skeletal muscle tissue, the surrounding
bones and muscles expand when the lungs expand resulting in the expansion of
the chest cavity. These bones and muscles consist of the ribs, the intercostals muscles between the ribs
and the main muscle of respiration the diaphragm
(a skeletal muscle that separates the chest from the abdominal cavity).
10.3a
Inspiration brings in air, expiration expels it
Air moves into
and out of the lungs in a cyclic manner.
Below is the general principle of gas pressure and
how these gases move
(Johnson 2012):
·
Colliding
molecules of gas cause gas pressure.
·
When
the volume of a closed space increases, the molecules of gas in that space are
farther away from each other, and the pressure inside the space decreases.
Conversely, when the volume in a closed space decreases, the gas pressure
increases.
·
Gases
flow from areas of higher pressure to areas of lower pressure.
Lungs cannot
contract or expand on their own. The pleural
cavity expands so will the lungs because they are stretchable.
Inspiration (inhalation) pulls air into the
respiratory system as lung volume expands and expiration (exhalation) pushes air out as lung volume declines
again.
Cycle of inspiration and expiration as follows (Oellers,
Online Presentation, 2012):
http://www.emc.maricopa.edu/faculty/farabee/biobk/biobookrespsys.html,
Retrieved April 13, 2012.
Inspiration (inhalation), when we
inhale our diaphragm contracts pulling muscles down, intercostal muscles
contract, elevates the chest wall and expands the volume of the chest, lowering
pressure in lungs, pulling in air.
Expiration (exhalation), when we
exhale muscles relax, diaphragm resumes dome shape; intercostals muscles allow
chest to lower, resulting in increase of pressure in chest and expulsion of
air.
10.3b Lung
volumes and vital capacity measure lung function
http://www.picsearch.com/imageDetail.cgi?id=JLqEzMTipb62juguPAWexxBqgQuIgTiS3aaFG_yT5kE&width=1663&start=1&q=respiratory%20center, Retrieved April 13, 2012.
Each breath you
take represents a tidal volume of air,
which is the total air, inhaled and exhaled in a single breath. Some of the air
we inhale will actually reach the alveoli and become involved in gas exchange;
the other will remain in the airways and is referred to as dead space volume.
The maximal volume that you can exhale
after a maximal inhalation is called your vital
capacity. Your vital capacity is almost 10 times your normal tidal volume
at rest. The amount of additional air that can be inhaled beyond the tidal
volume is called the inspiratory reserve
volume. Some air will always remain in your lungs this is called your residual volume.
A spirometer can measure your lung
capacity by having a person breathe normally into the device.
Lung volumes and
rates of change in volume are useful in diagnosing various lung diseases, like emphysema a condition where the smaller
airways lose elasticity, causing them to collapse during expiration and
impairing the ability to exhale naturally.
10.4 Gas
exchange and transport occur passively
Once the air
enters the alveoli, gas exchange and transport occur. There are basic
principles of governing the diffusion of gases to set the stage for external
and internal respiration (the second and third processes of respiration).
10.4a Gases
diffuse according to their partial pressures
Earth’s
atmosphere contains a mixture of gases: 78% nitrogen and 21% oxygen (Johnson
2012). In a mixture of gases, each gas exerts a partial pressure that is proportional to its percentage of the
total gas composition. Because partial pressures in a mixture of gases are
directly proportional to concentrations, a gas will always diffuse down its
partial pressure gradient, from a region of higher partial pressure to a region
of lower partial pressure (Johnson 2012). The exchange of oxygen and carbon
dioxide between the alveoli and the blood and between the blood and the tissues,
are passive. No ATP is used. The changes in partial pressures are used to
exchange and transport these gases.
10.4b External
respiration: The exchange of gases between air and blood
http://www.picsearch.com/imageDetail.cgi?id=hIghZAcvH28kd4KYqwIoBv3XSE4tUrqThOI4fAfDYv4&width=1663&start=1&q=partial%20pressure%20gas%20exchange, Retrieved April 14, 2012.
Oxygen diffused
from alveoli (104mmHg partial pressure) into the blood (40mmHg of partial
pressure), down its partial pressure gradient.
Carbon dioxide
diffuses from blood, which is 46mmHg partial pressure into the alveoli 40mmHg
partial pressure down its partial pressure gradient.
10.4c Internal
respiration: The exchange of gases with tissue fluids
http://www.picsearch.com/imageDetail.cgi?id=JLqEzMTipb62juguPAWexxBqgQuIgTiS3aaFG_yT5kE&width=1663&start=1&q=respiratory%20center, Retrieved April 12, 2012.
The body’s cells
get their supply of oxygen for cellular respiration from the interstitial fluid
that surrounds them. Because cells are constantly drawing oxygen from the
interstitial fluid (by diffusion), the interstitial fluid needs to be
replenished. This is accomplished by blood entering the capillaries. The oxygen
is then diffused into the interstitial fluid. Carbon dioxide is opposite, it
diffuses from the cell into the interstitial fluid and then into the capillary
blood (Johnson 2012).
Both external
and internal respiration occur entirely by diffusion. The partial pressure
gradients that permit diffusion are maintained by breathing, blood transport,
and cellular respiration (Johnson 2012). The end effect of all these processes
is that homeostasis of the concentrations of oxygen and carbon dioxide of the
cells is maintained.
10.4d Hemoglobin
transports most oxygen molecules
Oxygen is transported in blood in two ways (Johnson 2012):
1)
Bound
to hemoglobin in RBCs
2)
Dissolved
in blood plasma
http://www.picsearch.com/imageDetail.cgi?id=GeMm_8qZaU-ST7kmVlsCi-yedS0uNgSbo2YPf-_DK4s&width=1663&start=1&q=hemoglobin%20transporting%20oxygen%20and%20carbon%20dioxide, Retrieved April 14, 2012.
The
presence of hemoglobin is essential
for the transport of oxygen because oxygen is not soluble in water. Without
hemoglobin, the tissues would not be able to receive enough oxygen to sustain
life. 98% of oxygen in blood is carried bound to hemoglobin molecules in RBCs
(Oellers, Online Presentation 2012). 2% of oxygen is dissolved in plasma
(Oellers, Online Presentation, 2012).
Hemoglobin is a large
protein molecule consisting of four polypeptide chains, each of which is
associated with an iron-containing heme group that can bind oxygen (Johnson
2012). Oxyhemoglobin is formed because the four-heme groups bind four oxygen
molecules at a time.
This
is represented as:
Hb + O2 = HbO2
Hemoglobin Oxygen Oxyhemoglobin
This
formula is dependent on the partial pressures of oxygen in plasma. When the
partial pressure increases in the lungs, oxygen attaches to hemoglobin and is
transported in arterial blood (Johnson 2012). When the partial pressure
decreases at the tissues, oxygen detaches from hemoglobin.
Other factors
affect oxygen attachment to hemoglobin (Johnson 2012):
·
Binds
efficiently with a neutral pH
·
Cool
temperatures (similar to conditions in the lungs)
·
Affected
by carbon monoxide
10.4e Most
Carbon Dioxide is transported in plasma as bicarbonate
Cellular metabolism produces carbon
dioxide as a waste product. Blood is used to transport carbon dioxide away from
tissues and back to the lungs so that it can be removed. Carbon dioxide is
diffused into the blood by the tissues because the partial pressure of carbon
dioxide is higher in the tissues in the blood.
Carbon dioxide is transported in three ways (Johnson 2012):
1.
Dissolved
in blood plasma
2.
Bound
to hemoglobin
3.
In
the form of bicarbonate
Hemoglobin can
transport oxygen and carbon dioxide molecules at the same time because the two
gases attach to different sites.
Almost all
carbon monoxide produced by the tissues is converted to bicarbonate prior to
transport.70% of carbon dioxide is converted to and transported in the plasma
as bicarbonate which is used as a
buffer (absorbs and releases hydrogen to moderate pH. Bicarbonate from carbon
dioxide forms inside of RBCs, but quickly diffuses out of the RBCs and is
transported back to the lungs and dissolved in plasma.
Hydrogen ions
formed with the bicarbonate stay inside the RBCs and bind to hemoglobin. Their
attachment weakens the attachment between hemoglobin and oxygen molecules and
cause hemoglobin to release more oxygen. The presence of carbon dioxide
enhances the delivery of oxygen to the sites where it is most likely to be
needed.
As carbon
dioxide is removed by breathing, the bicarbonate and hydrogen ions formed in
the peripheral tissues to transport carbon dioxide are removed as well.
10.5 The nervous
system regulates breathing
Breathing
depends on contractions from the skeletal muscles that are activated by motor neurons.
Breathing is controlled by the nervous system, which regulates the rate and
depth of breathing to maintain homeostasis of carbon dioxide, hydrogen and
oxygen.
10.5a A respiratory
center establishes rhythm of breathing
http://www.google.com/#hl=en&sa=X&ei=Z2mLT8LDNoXm9ATb67nfCQ&ved=0CCoQvwUoAQ&q=picture+of+the+respiratory+center&spell=1&bav=on.2,or.r_gc.r_pw.r_qf.,cf.osb&fp=af73696fe4de10c7&biw=1680&bih=903,
Retrieved April 14, 2012.
The respiratory
center is positioned at the medulla
oblongata located in an area near the base of the brain and establishes
basic breathing patterns (Oellers, Online Presentation 2012). The respiratory center is a group of nerve
cells that automatically generate a cyclic pattern of electrical impulses every
4 to 5 seconds. These impulses stimulate the skeletal muscles to contract,
causing the rib cage to expand, the diaphragm to pull downward as we inhale. As
we inhale, the respiratory center receives sensory input from stretch receptors
in the lungs. These receptors monitor the degree of inflation of the lungs and
sever to limit inhalation and initiate exhalation. When the nerve impulses from
the respiratory center to the muscles end, the respiratory muscles relax, the
rib cage returns to its original size, the diaphragm moves upward again and we
exhale.
10.5b Chemical
receptors monitor carbon dioxide, hydrogen and oxygen levels
The body
modifies the rate and depth of breathing to maintain homeostasis. Under normal
circumstances the regulation of breathing centers to maintain homeostasis of
carbon dioxide, hydrogen and oxygen with the main emphasis on carbon dioxide
(Johnson 2012).
Certain cells in
the medulla oblongata detect changes in the hydrogen concentration of the cerebrospinal fluid (the interstitial
fluid around the cells in the brain). A rise in carbon dioxide increases
hydrogen and increases arterial blood. Receptor
cells detect elevated hydrogen concentrations and transmit signals to the
respiratory center, resulting in us breathing more frequently and more deeply,
exhaling more carbon dioxide and lowering blood levels of the gas back to
normal.
The aortic and carotid bodies are receptors
that detect changes in oxygen concentration in the arterial blood. If oxygen falls,
by at least 20% these receptors are activated and will signal the respiratory
center to increase the rate and depth of breathing in response to sufficiently
lowered arterial oxygen.
The rate and
depth of normal breathing is determined by the need to get rid of carbon
dioxide rather than the need to obtain oxygen (Oellers, Online Presentation,
2012).
10.5c We can
exert some conscious control
Conscious
control resides in the cerebral cortex. The ability to modify our breath gives
us the ability to speak and sing (Johnson 2012). We can even hold our breath
for a minute, but we are not able to override automatic regulatory mechanisms,
conscious control will be overpowered every time.
10.6 Disorders
of the respiratory system
Many factors can
lead to disorders of respiration like conditions that reduce airflow or gas
exchange, infections by microorganisms, cancer, diseases of other organs such
as congestive heart failure, and genetic diseases.
10.6a Reduced
air flow or gas exchange impedes respiratory function
Respiration depends on the flow of air between the
atmosphere and the alveoli and on the diffusional exchange of gases across the
alveolar and capillary walls. Any factor that impairs these activities impedes
respiratory function.
10.6a, 1 Asthma:
Spasmodic contraction of bronchi
Asthma is a spasmodic contraction of bronchial
muscle, bronchial swelling, and increased production of mucus (Johnson 2012).
An asthma attack causes partial closure of the bronchi, making breathing
difficult. Symptoms of an asthma attack include coughing while exercising,
shortness of breath, wheezing and a sense of tightness in the chest. Symptoms
can be triggered by viruses, air particles, allergies, exercise, tobacco smoke
and air pollution.
Most asthma
attacks are caused by a hyperactive immune system. When a person with asthma
breathes in allergens, the body reacts with excessive production of immunoglobulin
E. The IgE stimulates mast cells in the lungs, to release chemical weapons such
as histamine, leading to excessive inflammation and constriction of bronchiolar
smooth muscle.
Treatments focus
on preventing attacks by isolating the cause and avoiding it when possible.
10.6a, 2 Emphysema: Alveoli become
permanently impaired
http://www.picsearch.com/imageDetail.cgi?id=RcqsuUBmHVvCsh6Xx7qiwlYsXGfnTXh_6ZGgQYJ_KMU&width=1663&start=1&q=emphysema, Retrieved April 14, 2012.
Emphysema is a chronic disorder involving damage
to the alveoli (Johnson 2012). Connective tissue in the smaller airways is
destroyed resulting in airways that are less elastic, do not stay open properly
and tend to collapse during exhaling. The high pressures in the lungs damage
the fragile alveoli.
Most cases of
emphysema are associated with smoking or long-term exposure to air pollutants.
10.6b, 3
Bronchitis: Inflammation of the bronchi
Bronchitis refers to inflammation of the bronchi,
resulting in a persistent cough that produces large quantities of phlegm
(Johnson 2012). Bronchitis can be either acute or chronic depending on if you
smoke or live in a highly polluted area.
Symptoms include
wheezing, breathlessness and a persistent cough that yields yellowish or
greenish phlegm.
Acute bronchitis
can be treated by humidifying the lungs, drinking plenty of fluids, and taking
antibiotics if bacteria caused the infection.
10.6a, 4 Cystic
fibrosis: An inherited condition
Cystic fibrosis is an inherited condition in
which a single defective gene causes the mucus-producing cells in the lungs to
produce a thick, sticky mucus (Johnson 2012). This disease affects organ
systems. In the lungs, the thick mucus impedes airflow and provides a site for
bacteria to grow. Treatment includes physical therapy to try to dislodge the
mucus and keep the airways open.
10.6b
Microorganisms can cause respiratory disorders
Because the
lungs are moist, warm and covered in a thin layer of fluid they are prone to
infection. If microorganisms infect the lungs, serious diseases can be caused
like pneumonia, tuberculosis and botulism.
10.6b, 1 Colds
and the flu: Common viral respiratory tract infections
Viruses cause both colds and the flu. A cold is usually an upper respiratory
infection that includes symptoms like coughing, runny nose, nasal congestion
and sneezing. The flu is a virus of
the influenza family that include symptoms like a sore throat, fever and a
cough, sometimes accompanied by aches and chills, muscle pains, and headache.
There is no medical treatment for either of them. Rest and plenty of fluids are
the best prescription.
The same person
can catch colds and the flu repeatedly. The reason is that these viral
infections evolve rapidly, so that each year they are just a little bit
different from the previous year and so the immune system does not recognize
them.
10.6b, 2
Tuberculosis: Bacterial infection scars the lungs
Tuberculosis (TB) is an infectious disease caused
by the bacterium Mycobacterium tuberculosis. People pass the infection airborne
by sneezing or coughing. In most cases, the immune system fights off this
disease, but it can leave a scar on the lungs.
Symptoms include
coughing, chest pain, shortness of breath, fever, night sweats, loss of
appetite, and weight loss. A chest X-ray can reveal lung damage, such as
cavities in the lungs or old infections that have healed, leaving scarred lung
tissue. A skin test called the tuberculin
test can indicate whether someone has been exposed to the infection.
10.6b, 3
Botulism: Poisoning by bacterial toxin
Botulism is a form of poisoning caused by a
bacterium, Clostridium botulinum, occasionally found in improperly cooked or
preserved foods (Johnson 2012). This bacterium produces a toxin that blocks the
transmission of nerve signals to skeletal muscles, including the diaphragm and
intercostals muscles.
Symptoms will
appear 8 to 36 hours after eating contaminated food. You may have a hard time
swallowing and speaking, double vision, nausea, and vomiting.
If botulism is
not treated, it can be fatal because it paralyzes the respiratory muscles.
10.6c Lung
cancer is caused by proliferation of abnormal cells
http://www.picsearch.com/imageDetail.cgi?id=LmO3zE2bGjmmtyoA6fTi3L-EZQfP9Fqe5mb22QDRzbw&width=1663&start=1&q=lung%20cancer, Retrieved April 14, 2012.
Cancer is the uncontrolled growth of abnormal
cells (Johnson 2012). Cancer in the lungs impair the normal function of the
lungs and can impair the movement of air in the airways, exchange of gases in
the alveoli and the flow of blood in pulmonary blood vessels.
Lung cancer
takes years to develop and is associated with smoking. Symptoms include chronic
cough, wheezing, chest pain and coughing up blood. Lung cancer is highly
preventable if you do not smoke, know the conditions of your work environment,
and have your home inspected for radon gas.
10.6d
Pneumothorax and atalectasis: A failure of gas exchange
A pneumothorax is collapse of one or more lobes
of the lungs (Johnson, 2012). The most common cause is a penetrating wound of
the chest that allows air into the pleural cavity around the lungs, but can
also occur because of disease or injury to a lung. Pneumothorax can be life
threating because of the inability to inflate the lungs, which results in a reduced
exchange of oxygen and carbon dioxide.
Treatment
requires repairing the damage to the chest wall or lungs and removing the air
from the pleural cavity.
Atalectasis refers to a lack of gas exchange within
the lung because of alveolar collapse or a buildup of fluid within alveoli
(Johnson 2012). This can be caused by a complication of surgery or the amount
of surfactant is deficient.
Treatment
involves finding and reversing the underlying cause.
10.6e Congestive
heart failure impairs lung function
Congestive heart failure is a
cardiovascular condition in which the heart gradually becomes less efficient
and can eventually impair lung function.
Congestive heart failure begins when the heart
fails as a pump, this can cause high blood pressure, increase the diffusional
distance and reduces diffusion of gases.
Treatments focus
on reducing this fluid buildup by helping the body get rid of fluid and
improving the heart’s pumping action.
REFERENCES
Johnson, M. D. (2012, 2010, 2008).
Human Biology: concepts and current issues, sixth edition. Pearson Education,
inc.; Benjamin Cummings.
Oellers, J. (n.d). Online
Presentation: Ch. 10 The Respiratory System: Exchange of gases. Retrieved April
14, 2012, from http://lblackboard.yc.edu/webapps/portal/frameset.jsp?tab_tab_group_id=_2_1&url=%2Fwebapps%2Fblackboard%2Fexecute%2Flauncher%3Dcourse%26id%3D_43466_1
Science News (April 13, 2012).Implantable
medical device is designed to warn patients of impending heart attack.
Retrieved April 14, 2012 from http://www.sciencedaily.com/releases/2012/04/120413145305.htm

















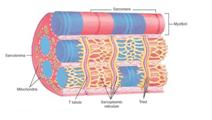



























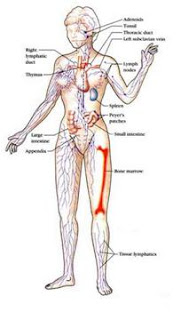



























No comments:
Post a Comment